
PROFESSIONAL DEVELOPMENT PAPER
NSGC Practice Guideline: Prenatal Screening and Diagnostic
Testing Options for Chromosome Aneuploidy
K. L. Wilson & J. L. Czer winski & J. M. Hoskovec &
S. J. Noblin & C. M. Sullivan & A. Harbison &
M. W. Campion & K. Devary & P. Devers &
C. N. Singletary
Received: 1 June 2012 / Accepted: 17 September 2012 / Published online: 22 November 2012
#
National Society of Genetic Counselors, Inc. 2012
Abstract The BUN and FASTER studies, two prospec-
tive mult icenter trials in the United States, validated the
accuracy and detection rates of first and second trimester
screening previously reported abroad. These studies, cou-
pled with the 2007 release of the American College of
Obstetricians and Gynecologists (ACOG) Practice Bulle-
tin that endorsed first trimester screening as an alternative
to traditional s econd trimester multiple m arker screening,
led to an explosion of screening options available to
pregnant women. ACOG also recommended that invasive
diagnostic testing for chromosome aneuploidy be made
available to all women regardless of maternal age. More
recently, another option known as Non-invasive Prenatal
Testing (NIPT) became available to screen for chromo-
some aneuploidy. While screening a nd test ing opt ions
may be lim ited due to a variety of fact ors, healthcare
providers need to be aware of the options in their area
in order to provide their patients with accurate and reli-
able information. If not presented clearly, patients may
feel overwhelmed at the number of choices available. The
following guideline includes recommendations f or health-
care providers regarding which sc reening or diagnostic
test should be offered based on availability, insurance
coverage, a nd ti ming o f a patient’s entry into prenatal
care, as well as a triage assessment so that a ge neral
process can be adapted to unique situations.
Keywords Prenatal screening
.
Prenatal testing
.
Chromosome aneuploidy
.
Genetic counseling
.
National
Society of Genetic Counselors
.
Practice guidelines
Purpose
To provide information that assists physicians and allied health
professionals in making decision s about diff erent screening and
diagnostic testing for chromosome aneuploidy throughout
pregnancy.
K. L. Wilson (*)
Department of Ob/Gyn, Division of Gynecologic Oncology,
The University of Texas Health Science Center at Houston,
6410 Fannin St, Suite 1217,
Houston, TX 77030, USA
e-mail: [email protected]
S. J. Noblin
:
C. N. Singletary
Department of Pediatrics,
The University of Texas Health Science Center at Houston,
6410 Fannin Street, Suite 1217,
Houston, TX 77030, USA
P. Devers
Department of Obstetrics and Gynecology,
Division of Maternal-Fetal Medicine,
University of North Carolina at Chapel Hill,
CB# 7516,
Chapel Hill, NC 27599-7516, USA
A. Harbison
Deparment of Ob/Gyn, Division of Maternal
Fetal Medicine, The University of Texas
Health Science Center at Houston,
5656 Kelley Street,
Houston, TX 77026, USA
M. W. Campion
Boston University School of Medicine,
85 E. Newton St, M913,
Boson, MA 02118, USA
K. Devary
EvergreenHealth Maternal Fetal Medicine,
12333 NE 130th Lane, Suite Tan 240,
Kirkland, WA 98034, USA
J. L. Czerwinski
:
J. M. Hoskovec
:
C. M. Sullivan
Department of Ob/Gyn, Division of Maternal Fetal Medicine,
The University of Texas Health Science Center at Houston,
6410 Fannin St, Suite 1217,
Houston, TX 77030, USA
J Genet Counsel (2013) 22:4–15
DOI 10.1007/s10897-012-9545-3

Disclaimer
The practice guidelines of the National Society of Genetic
Counselors (NSGC) are developed by members of the NSGC
to assist genetic counselors and other health care providers in
making decisions about appropriate management of genetic
concerns; including access to and/or delivery of services. Each
practice guideline focuses on a clinical or practice-based issue,
and is the result of a review and analysis of current profes-
sional literature believed to be reliable. As such, information
and recommendations within the NSGC practice guidelines
reflect the current scientific and clinical knowledge at the time
of publication, are only current as of their publication date,
and subject to change without notice as advances emerge.
In addition, variations in practice, which take into account
the needs of the individual patient and the resources and
limitations unique to the institution or type of practice, may
warrant approaches, treatments, and/or procedures that differ
from the recommendations outlined in this guideline. There-
fore, these recommendations should not be construed as dic-
tating an exclusive course of management, nor does the use of
such recommendations guarantee a particular outcome. Ge-
netic counseling practice guidelines are never intended to
displace a health care provider’s best medical judgment based
on the clinical circumstances of a particular patient or patient
population. Practice guidelines are published by NSGC for
education and informational purposes only, and NSGC does
not “approve” or “endorse” any specific methods, practices, or
sources of information.
Background
The landscape of prenatal screening changed in 2007 with
the release of two ACOG Practice Bull etins stating all
women should be offered maternal serum screening (MSS)
and diagnostic testing regardless of maternal age, and that
healthcare provide rs should determine which screening
options would best serve their patients (ACOG Practice
Bulletin No. 77 & 88, 2007). ACOG’s assertion was subse-
quently echoed by the American College of Medical Genet-
ics (ACMG), leaving providers to reassess their screening
and diagnostic testing practices (Driscoll and Gro ss 2008).
Prenatal screening strategies have evolved greatly over the
years. Various combinations of firs t and second trimester
maternal serum analytes and fetal ultrasound findings have
been proposed as part of an ongoing quest to create a screen-
ing test with the highest detection and lowest false positive
rates. Recently, NIPT has been made commercially available
as an alternative option for chromosome aneuploidy screen-
ing. Screening options for chromosome aneuploidy are non-
invasive, which may make them attractive options for patients
who desired more individualized risk assessment information
prior to making a decision about whether or not to undergo
invasive diagnostic testing. The primary limitation of screen-
ing is that it does not provide a definitive diagnosis, leading to
the potential of increased anxiety in women with an unaffect-
ed pregnancy and the potential of false reassurance in women
who have a pregnancy with a chromosome aneuploidy. An-
other limitation of screening is the variability in the detection
rates, false positive rates, screening cut-offs, and anatomical
ultrasound markers included in the screen based on the par-
ticular laboratory and/or provider involved. In addition, detec-
tion rates for screening in multiple gestations are generally
decreased from those of singletons (Wald and Rish 2005). For
a more comprehensive review of the advantages and limita-
tions of the types of screening, refer to the individual sections
below and to Tables 1, 2,and3. A decision tree to assist
providers in selecting a screening method that is most suitable
for their practice is presented in Fig. 1.
In addition to the various prenatal screening options, diag-
nostic testing for chromosomal abnormalities (Table 4)is
available. Chorionic villus sampling, or CVS, is typically
performed between 10-13w6d of gestation, and involves a
transcervical or transabdominal aspiration of chorionic villi
from the developing placenta (Wapner 2005). Another option
for diagnostic testing is amniocentesis. Amniocentesis is tra-
ditionally performed after 15 weeks of gestation by trans-
abdominal removal of amniotic fluid (CDC 1995). Samples
obtained through CVS and amniocentesis are typically used
for chromosomal analysis by karyotyping, but may also be
used for rapid interphase fluorescence in situ hybridization
(FISH) to screen for chromosome aneuploidy, metaphase
FISH to evaluate for specific microdeletions or microduplica-
tions, chromosomal microarray, or other molecular testing.
A referral for genetic counseling has traditionally been
made for patients who have an increased risk for chromosome
aneuploidy, including those with a positive maternal serum
screen result, positive family history, a fetal anomaly identi-
fied on ultrasound, or those who are 35 years of age or older at
delivery. However, as screening options have expanded, it has
become more routine to refer patients for genetic counseling
when they are having difficulty deciding on a course of action
for screening or diagnostic testing. Appropriate screening and
diagnostic testing options are typically presented to patients in
the context of a prenatal genetic counseling session (CDC
1995). Genetic counselors are uniquely trained to explain
complex information in an understandable format to patients
and to facilitate the informed decision-making process.
First Trimester Screening Options
The first trimester analyt es pregnancy associa ted plasma
protein-A (PAPP-A) and free beta-human chorionic gonad-
otropin (β-hCG) may be measured between 9w0d-13w6d of
gestation, while the nuchal translucency (NT) measurement
NSGC Practice Guideline 5

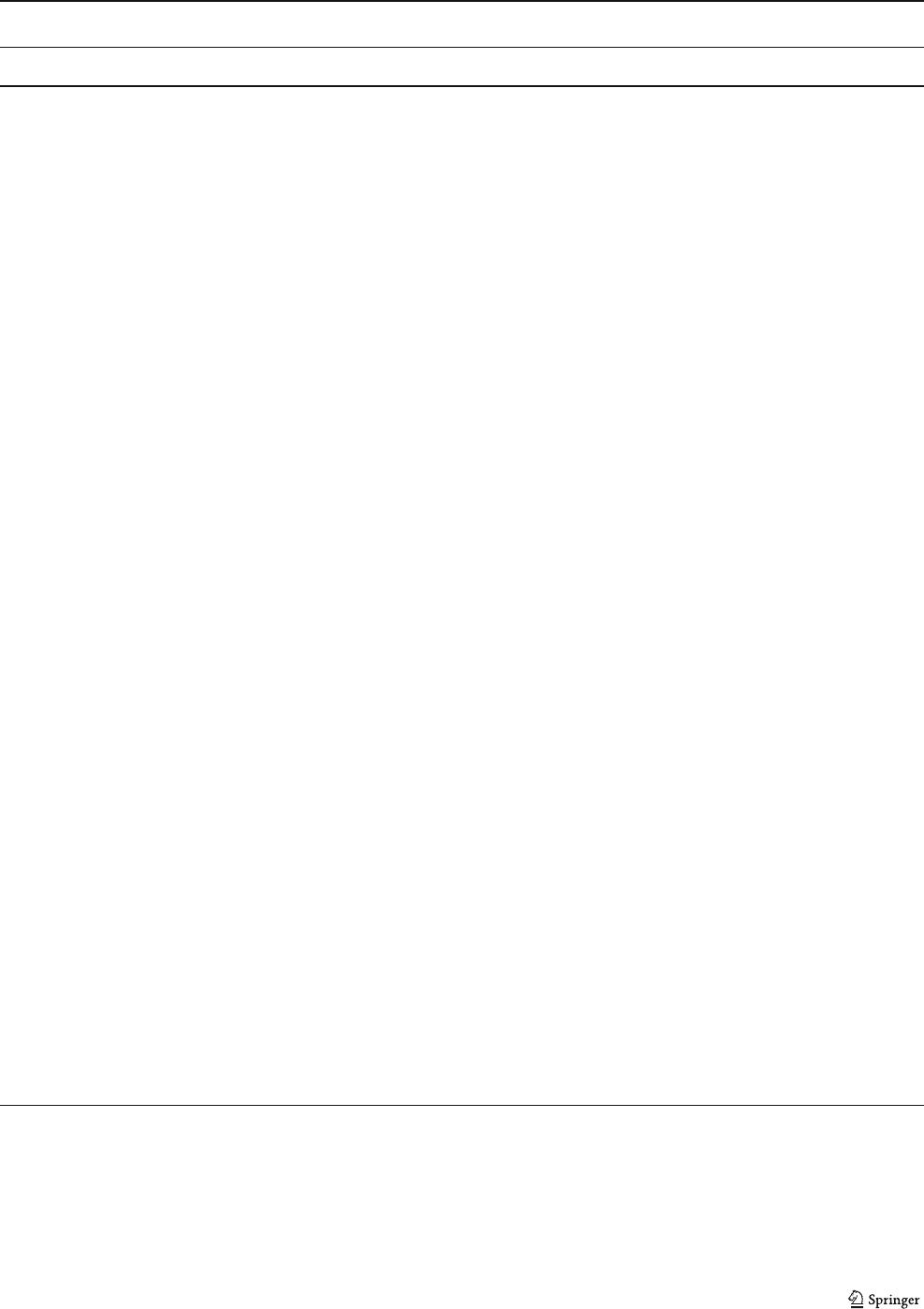
Table 1 Screening options for chromosome aneuploidy in pregnancy
First
Trimester
Analyte
Combined
First
Trimester
Integrated Serum Integrated Stepwise
Sequential
Contingency Multiple
Marker
Serum
Screening
9
Non Invasive
Prenat al
Testing
First
visit
Second
visit
6
First visit Second
visit
6
First visit Second
visit
7
First visit Second
visit
7
Gestational
Age at
Blood Draw
9w0d-
13w6d
9w0d-
13w6d
9w0d-
13w6d
15w0d-
21w6d
9w0d-
13w6d
15w0d-
21w6d
9w0d-
13w6d
15w0d-
21w6d
9w0d-
13w6d
15w0d-
21w6d
15w0d-
21w6d
10w0d -
21w6d
Maternal
Serum
Analytes
PAPP-A
b-hCG
(or hCG)
1
PAPP-A
b-hCG
(or hCG)
1
PAPP-A AFP
hCG
uE3
DIA
PAPP-A AFP
hCG
uE3
DIA
PAPP-A b-hCG
(or hCG)
1
AFP
hCG
uE3
DIA
PAPP-A b-hCG
(or hCG)
1
AFP
hCG
uE3
DIA
AFP
hCG
uE3
DIA
ITA
9
Circulating
Cell Free
Fetal DNA
10
NT Utilized No Yes
4
Yes
4
No Yes
4
Yes
4
No No
Down Syndrome
Detection Rate
62–63 %
2
78–91 %
2
n/a
5
94–96 %
2
n/a
5
87–88 %
2
91–95 %
2
91–92 %
2
75–83 %
2
99–100 %
11, 12
Trisomy 18
Detection Rate
82 %
3
91–96 %
3
n/a
5
91–96 %
3
n/a
5
82 %
3
91–96 %
3
91–96 %
3
60–70 %
3
97–100 %
11, 12
Provides
ONTD Risk
No No n/a
5
Yes n/a
5
Yes No Yes
8
No Yes
8
Yes No
•Sources: Barkai et al. (1993); Bianchi et al. (2012); Cole et al. (1999); Cuckle et al. (2008); Haddow et al. (1998); Malone et al.(2005); Norton et al. (2012); Palomaki et al. (2006); Palomaki et al.
(2012); Spencer and Nicolaides (2002); Wald et al. (2003); Wald et al. (2004); Wapner et al. (2003)
1. Whole molecule hCG used in place of free b-hCG by some laboratories and some laboratories add additional analytes such as DIA, both of which may change detection rates
2. Typically at 5 % false positive rate (FPR) with 1/270 cut-off for screen positive; if other FPR or cut-off used, may change detection rate; FPR averages 15–20 % if AMA
3. Typically at 0.5 % FPR with 1 in 100 cut-off, if other FPR or cut-off used, may change detection rate; some laboratories quote combined t18/t13 risk & detection rate
4. The timing of assessment for the NT measurement is between 10w4d and 13w6d
5. Results not provided after first visit
6. Second blood draw is required for all patients
7. Second blood draw is indicated for a portion of patients after the first step of the screen, but not all patients
8. NTD risk assessment is performed for those patients who need a second step and thus get a blood draw that contains AFP as an analyte
9. ITA is included by one laboratory along with AFP, hCG, uE3, and DIA and referred to as the Penta Screen; detection rates are similar to the Quadruple Screen
10. Cell free fetal DNA is found in maternal blood but is not considered an analyte like traditional serum screening
11. While initial studies show a range of detection rates up to 100 % for trisomy 18 & 21, NIPT is not yet considered diagnostic and follow-up CVS or amnio is recommended for a positive NIPT
12. Typically <1 % FPR (from 0.1 to 0.97 %); laboratories generally report trisomy 13 as well, with detection ranging 79-92% at <1 % FPR.
6 Wilson et al.
is valid when measured between 10w4d-13w6d of gestation.
It is important to note that some laboratories substitute hCG
for β-hCG, which may impact detection rates. Most labora-
tories target a 5 % false positive rate for serum screening
options.
There are three options for first trimest er screening. NT
only with maternal age relies upon the size of the fetal NT
and the patient’s age to calculate a risk estimate. First
trimester analyte screening relies upon the levels of mater-
nal serum PAPP-A and free β-hCG or total hCG combined
Table 2 Aneuploidy screening options comparison table
Advantages Limitations Physician likely to utilize screen
First
Trimester
Analyte
Screening
• 1st trimester result
• NT not required
• 1 visit
• CVS is an option if screen positive
• Lower detection rate compared to other
screening options that include NT
Physician with an early-to-care patient
population who does not have access
to a certified NT provider, but does
have access to CVS, and prefers to
complete screening in one visit.
Combined
First
Trimester
Screening
• 1st trimester result
• 1 visit
• CVS is an option if screen positive
• NT required
• Lower detection rate compared to integrated
screen
Physician with an early-to-care patient
population who has access to certified
NT provider and to CVS, and prefers
to complete screening in one visit.
Integrated
Screening
• Highest detection rates out of all of
maternal serum screening tests
• 2 visits
• NT required
• Results given in 2nd trimester
Physician with an early-to-care patient
population who has access to certified
NT provider, but does not have access
to CVS.
Serum
Integrated
Screening
• Highest detection rates for screening
when the NT is not available
• NT not required
• 2 visits
• Results given in 2nd trimester
• Lower detection rate compared to screens that
include NT, such as integrated screen
Physician with an early-to-care patient
population who does not have access
to certified NT provider or to CVS.
Stepwise
Sequential
Screening
• 1st trimester result for highest risk
patients allows option of CVS
• Detection rate higher than combined
FTS while still allowing for some 1st
trimester results
• 2 visits for most patients
• NT required
• Lower detection rate compared to integrated
screen
Physician with an early-to-care popu-
lation and high follow-up compliance
who has access to a certified NT pro-
vider and to CVS, who wants infor-
mation early enough to offer CVS if
risk is high, and wants to avoid mod-
erate risk group created by contingency
screening.
Contingency
Screening
• 1st trimester results for high and low
patients, minimizing number of patients
needing a second visit
• 2 visits for moderate risk group
• NT required
•
Initial moderate risk group may not feel as
reassured with 2nd trimester negative screen
results as initial low risk group
Physician with an early-to-care patient
population and high follow-up com-
pliance who has access to a certified
NT provider and to CVS, and who
feels the benefit of a one visit screen
for most patients outweighs anxiety
caused for patients who fall into the
moderate risk group and are later re-
stratified to a low-risk group.
Multiple
Marker
Serum
Screening
• Allows for screening in women
presenting for care after the first
trimester
• 1 visit
• Results given in 2nd trimester
• Lower detection rate compared to screens that
include first trimester components and/or NT
Physician who has patients who
present primarily in second trimester
for screening or patients whose
insurance does not cover NT screening.
Non Invasive
Prenatal
Testing
• 1st or 2nd trimester result in 1 visit
without NT required
• Highest detection rates across all non
invasive options
• New technology with shorter publication
history and less information on payer coverage
Physician comfortable with new
technology who wants a screening test
with high detection rate and low false
positive rate that can be applied in
both first and second trimester.
NSGC Practice Guideline 7
with maternal age for risk estimation. The third method is
referred to as combined first trimester screening, because it
combines the use of the NT meas urement, the first trimester
maternal serum analytes (PAPP-A, and free β-hCG or total
hCG) and maternal age. Combined first trimest er screening
has been demonstrated to have higher detection rates for
Down syndrome (78–91 %) and trisomy 18 (91–96 %)
compared to NT only or serum analyte only m etho ds
(Malone et al. 2005;Waldetal.2003;Wapneretal.
2003), (Refer to Tables 1 and 3). Some studies have
reported that pregnancies affected with trisomy 13 have
an analyte and NT pattern sim ilar to tri somy 18; thus, it
may also be possible to use combined first trimester
screening to screen for trisomy 13 (Spencer et al. 2000).
When the NT measurement is significantly elevated (typi-
callyconsideredtobeanNT≥3.0 mm or the 95th percentile),
the possibility of chromosome aneuploidy is significantly
increased, and it is appropriate to offer the option of diagnostic
testing at that point without performing or waiting for the
results of the MSS (Comstock et al. 2006). In addition to
chromosome aneuploidies, NT ≥3.5 mm is also associated
with an increased risk of a congenital heart defect. In such
cases, fetal echocardiography is recommended during the
second trimester. It is important to note that once an elevated
NT is seen, the risk for an adverse pregnancy outcome remains
increased even if normal fetal karyotype is confirmed (Bilardo
et al. 2010).
As none of the first trimester screening options allow for
a calculation of the risk for open neural tube defects
(ONTD), a maternal serum alpha-fetoprotein (MSAFP)
sample should be drawn in the second trimester in patients
undergoing first trimester screening. ONTDs may also be
detected on second trimester ultrasound. It is not recom-
mended that an independent risk assessment for chromo-
some aneuploidy be performed in both the first and second
trimesters due to the high false positive rate (Platt et al.
2004).
The presence or absence of the fetal nasal bone and of
tricuspid regurgitation on first trimester ultrasound have
been proposed as additional ultrasound markers for chromo-
some aneuploidy (Kagan et al. 2009 ; Ozkaya et al. 2010).
However, at the present time, the use of these anatomical
markers to determine chromosome aneuploidy risk is not
universally recommended.
Non-Invasive Prenatal Testing (NIPT) NIPT uses circulat-
ing cell free fetal DNA in maternal plasma to evaluate for
Down syndrome, trisomy 18, and trisomy 13. Published
studies show a low false posit ive rate (<1 %) and a very
high detection rate for Down syndrome (99–100 %), triso-
my 18 (97–100 %) and trisomy 13 (79 – 92 %), (Bianchi et
al. 2012; Norton et al. 2012; Palomaki et al. 2012), (see
Table 1). In addition, Bianchi et al. fo und a 94 %
detection rate for monosomy X and reported several
Table 3 Ultrasound screening options for aneuploidy
Nuchal Translucency FetalAnatomy Ultrasound
Gestational Age 10w4d–13w6d 18w0d–20w6d (ideal)
16w0d–24w6d (at some centers)
Ultrasound Markers
Evaluated
Increased Nuchal
Translucency
1,2
Structural Defects, e.g., congenital heart defects, hydrocephalus, holoprosencephaly, cystic
hygroma, cleft lip, duodenal atresia, omphalocele, kidney malformations, intrauterine growth
restriction, clenched hands, etc.
4
Soft Markers, e.g., increased nuchal fold, choroid plexus cyst, echogenic bowel, hydronephrosis,
echogenic focus/foci, single umbilical artery, clinodactyly of the 5th finger, shortened long bones
4
Down Syndrome
Detection Rate
60–82 %
3,4
50–70 %
4,5
Trisomy 18
Detection Rate
71–82 %
3,4
80%
4,5
Provides ONTD
Risk Assessment
No Yes
•Sources: ACOG, 2009; Malone et al. 2005; Nicolaides et al. 2002; Nyberg and Souter 2001; Sanders et al. (2002); Taslimi et al. 2005; Wald et al.
2003; Wapner et al. 2003
1. Defined as>95th percentile or >3.0 mm by the majority of studies
2. Other ultrasound markers such as nasal bone and tricuspid regurgitation remain early in investigation and are not included
3. False positive rate 20–25 %; includes age in detection rate; without age detection is lower
4. Detection rate is affected by gestational age, quality of ultrasound images, operator experience, equipment used, referral indication, criteria for
positive findings, maternal habitus and fetal position
5. Adjustment of a priori risk based on the association between a given ultrasound finding and aneuploidy varies by center. The magnitude of
increased risk is impacted by the specific findings and the strength of their association with aneuploidy
8 Wilson et al.

ca ses of mosaicism for trisomy 21, trisomy 18, and mono-
somy X (2012). The landmark NIPT studies recruited
women who were otherwise pursuing i nvasive testing.
Thus, the major ity were from high-risk populations that
had an increased risk to have a fetus affected with chromo-
some aneuploidy. At this time, NIPT is only recommended for
patients from high-risk populations, including advanced ma-
ternal age, positive screening test, abnormal ultrasound sug-
gestive of aneuploidy, or prior pregnancy with chromosome
aneuploidy (Devers et al. 2012). It is recomme nded t hat a
positive NIPT be followed by confirmatory diagnostic
testi ng prior t o making pregnancy decisions (Benn et al.
2011; Devers e t al. 2012). NIPT is validated between
10w0d–21w6d gestation, making it an option for wom-
en that present in either the first or the second trimester.
Many practices are using NIPT in addition to their
already established screening practices to provide high-
risk patients with m ore information prior to m aking a
decision about invasive diagnostic testing. If NIPT is
performed, additional serum screening for chromosome
aneuploidy is not recommended. While NIPT has prom-
ise for the future and may potentially replace other
screening methods as the standard of care, there is s till
much to learn about this technology and its clinical
utility. For more information regarding N IPT, please refer
to the fact sheet published in 2012 by the National
Coalition for Health Professional Education in Genet ics
and NSGC.
Integrated, Serum Integrated, Stepwise Sequential
and Contingency Screening
Screening strategies that combine both first and second
trimester serum analytes and ultrasound markers have been
proposed as a means of increasing detection rates while
decreasing false positive rates. Since these screening options
involve multiple steps, it may be difficult to ensure that all
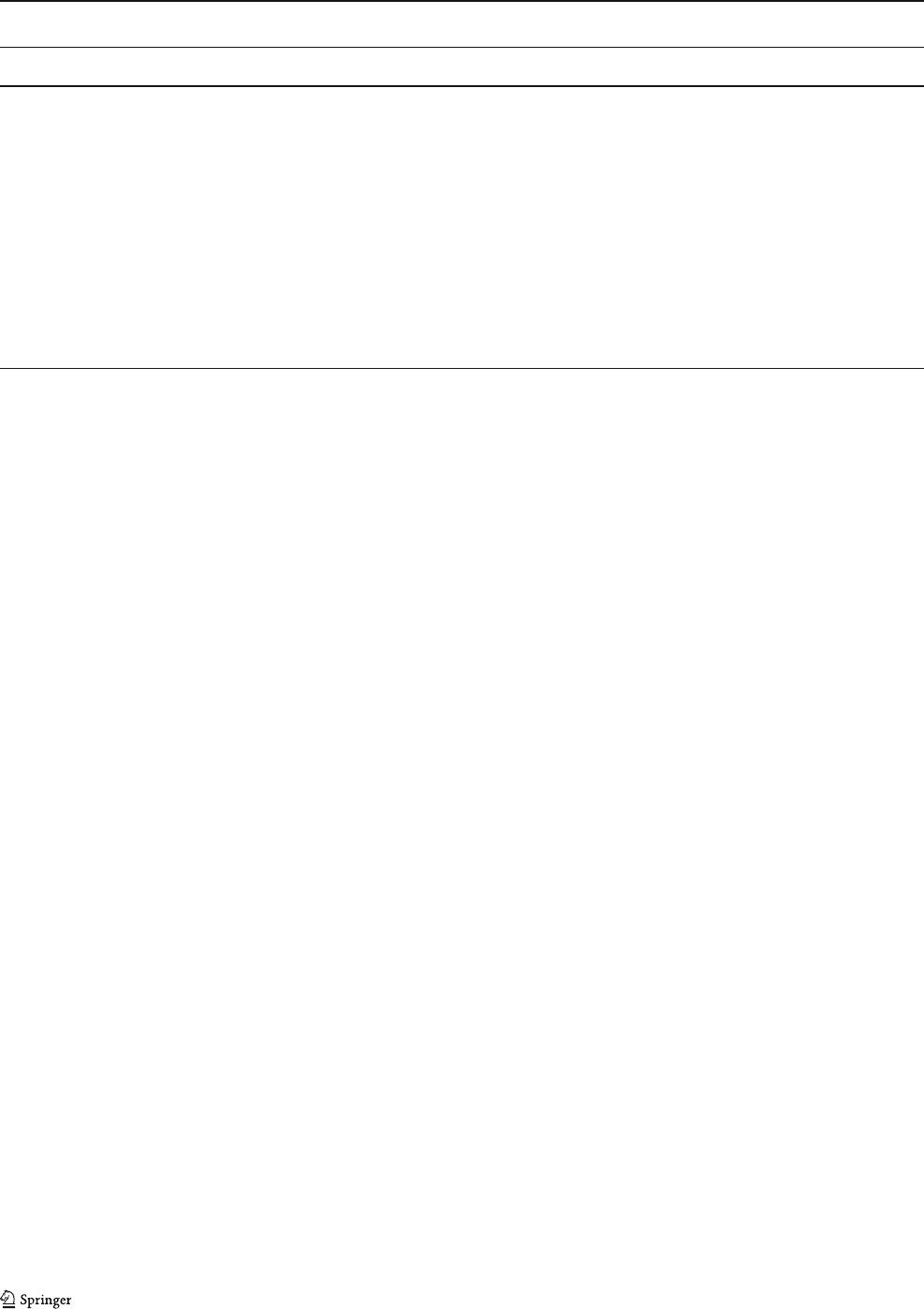
Following appropriate counseling, does patient
wish to pursue prenatal screening or testing?
YES
Patient elects
1
diagnostic testing
Chorionic
Villus
Sampling
between
10 and 13
weeks
Amnio -
centesis
>15 weeks
Patient elects screening
2
prior
to making a decision about
diagnostic testing
Patient fits current
criteria for NIPT &
elects NIPT
NIPT
1
st
or 2
nd
trimester
result
1 visit
Patient elects maternal
serum screening
< 14
weeks
NT
3
NOT
available/feasible
First
Trimester
Analyte
1
st
trimester
result
1 visit
Serum
Integrated
2
nd
trimester
result
2 visits
NT
3
available/feasible
Combined
FTS
1
st
trimester
result
1 visit
Stepwise
Sequential
1
st
trimester
result if very
high risk
2
nd
trimester
result if less
risk
1-2 visits
Integrated
2
nd
trimester
result
2 visits
Greatest
analyte
detection
rate
Contingency
1
st
trimester
result if high or
low risk
2
nd
trimester
result for
moderate risk
1-2 visits
> 14
weeks
Quadruple
Marker
Screening
1 visit
NO
1
See Table 4 for more information about diagnostic testing.
2
See Table 1 for more information about screening options.
3
NT= Nuchal translucenc
y
Fig. 1 Decision tree for selecting between screening and diagnostic testing options
NSGC Practice Guideline 9
patients return for the multiple visits required to complete
the screen ing process (Wald et al. 2003).
Integrated Screening uses a two-step process to adjust the
maternal age-related risk for Down syndrome and trisomy
18. The first step involves NT and PAPP-A measurements in
the first trimester, and the second step involves serum analyte
measurements of AFP, hCG, unconjugated estriol (uE3), and
dimeric inhibin A (DIA) in the second trimester (Cuckle et al.
2008;Maloneetal.2005;Waldetal.2003). The patient is
given a single risk assessment after both steps have been
completed. Integrated screening has a high detection rate for
Down syndrome (94–96 %) and trisomy 18 (91–96 %); how-
ever , patients must wait until the second trimester for results,
which eliminates the opportunity for early diagnostic testing
such as CVS (Malone et al. 2005; Spencer and Nicolaides
2002;Waldetal.2004;Wapneretal.2003). When an NT
measurement is not possible, serum integrated screening may
still be performed at a lower detection rate for Down syndrome
(87–88 %) and trisomy 18 (82 %), (Malone et al. 2005;Wald
and Rish 2005;Wapneretal.2003).
Stepwise Sequential Screening also involves two steps,
with the first step combining the NT measurement, serum
analytes PAPP-A and β-hCG (or hCG), and maternal age in
the first trimester. Patients are initially stratified into a
“high” or “low” risk group as determined by the screening
laboratory’s risk cut-off figures. These initial results are
disclosed to patients who fall into the high risk group, and
they are subsequently offered diagnostic testing. Initial results
may or may not be disclosed to patients who fall into the low
risk group, and they proceed with a second blood draw per-
formed in the second trimester. In this second step, the serum
analytes AFP, hCG, uE3, and DIA are incorporated into the
risk assessment, and the patient is given a risk for chromo-
some aneuploidy based on the combined results of both of the
screening steps. The overall detection rate for stepwise se-
quential screening is 91–95 % for Down syndrome and 91–
96 % for trisomy 18 (Malone et al. 2005;Palomakietal.2006;
Spencer and Nicolaides 2002; Wapner et al. 2003). Stepwise
sequential screening allows the patients with the highest risk
to consider diagnostic testing in the first trimester of pregnan-
cy while retaining some of the increase in detection rates seen
with integrated screening.
Contingency Screening is another two-step screening option.
As with stepwise sequential screening, the first step adjusts
maternal age-related risk for chromosome aneuploidy based
on the NT measurement and serum analytes. However , after
the first step, patients are divided into low, moderate, and high
risk groups based on their risk assessment for chromosome
abnormality. The high risk group is offered diagnostic testing,
the moderate risk group continues to the second serum analyte
screening step, and the low risk group is not offered further
serum analyte screening. Once the moderate risk group under-
goes second trimester analyte screening (AFP, hCG, uE3, and
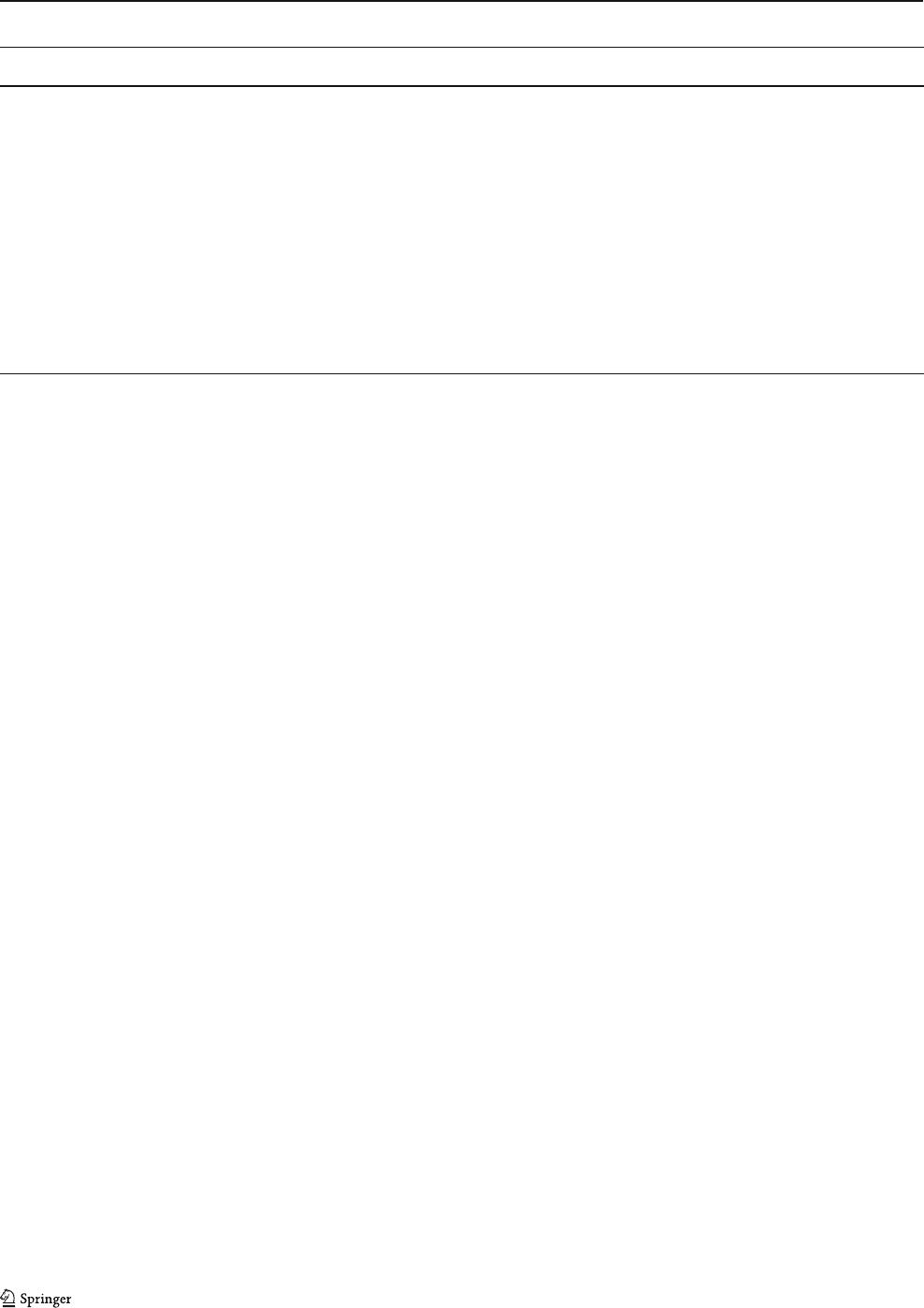
Table 4 Diagnostic testing options
Chorionic Villus Sampling (CVS) Early Amniocentesis
4
Amniocentesis
Gestational Age at
Time of Procedure
1
10w0d–13w6d 11w0d–13w0d 15w0d–23w6d
Test Methodology Transcervical or transabdominal
aspiration of chorionic villi from
developing placenta
Abdominal withdrawal of amniotic
fluid from gestational sac
Risk of Miscarriage 0.5–1.0 % 2.0 % 0.2–0.3 %
5
Additional Associated Risks
2
• Mosaicism: <1 % • Mosaicism: 0.2 % • Mosaicism: 0.2 %
• Maternal Cell Contamination: <1 % • Club foot: 1.3% –1.7 % • Club foot:<0.1 %
• Spotting & Cramping: 15 % • Amniotic Fluid Leakage:
3.5 % – 4.4 %
• Amniotic Fluid Leakage: 1.7 %
Down Syndrome Detection Rate
3
98–99 % 99.80 % 99.90 %
Trisomy 18 Detection Rate
3
98–99 % 99.80 % 99.90 %
Provides ONTD Detection No Yes Yes
Sources: ACOG Practice Bulletin No. 88, 2007; Brambati et al. 1992; Canadian Collaborative CVS Amniocentesis Clinical Trial Group, 1989;
Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report, 1995; Eddleman et al. 2006; Jackson et al. 1992; Ledbetter et
al. 1992; Sundberg et al. 1997; The Canadian Early and Mid-trimester Amniocentesis Trial Group, 1998; Wapner et al. 2003; Winsor et al. 1999
1. May be performed at other gestational ages, but risks and benefits may vary
2. An increased risk for limb reduction defects has been associated with CVS performed prior to 10 weeks gestation
3. Detection rates based on karyotyping; other detection rates may apply when utilizing fluorescence in situ hybridization or chromosomal
microarray
4. Early amniocentesis is not recommended by ACOG
5. Range of 0.06–1.0 % [or 1 in 1600 to 1 in 100] reported in literature
10 Wilson et al.

DIA), these patients are then stratified again into a high risk
group who is offered diagnostic testing and a low risk group
who is not considered at great enough risk to warrant diagnostic
testing. The overall detection rate for contingency screening
when both steps are performed is 91–92 % for Down syndrome
and 91–96 % for trisomy 18 (Cuckle et al. 2008;Palomakietal.
2006; Spencer & Nicolaides 2002;Wapneretal.2003). Con-
tingency screening lowers the number of patients proceeding to
the second trimester serum analyte screening step compared to
stepwise sequential screening, while still identifying the major-
ity of high risk pregnancies in the first trimester. However,
patients identified as initially having a moderate risk may retain
some anxiety even if the second step places them back into the
low risk group.
Second Trimester Screening Options
Second trimester MSS options include the triple screen, the
quadruple (quad) screen, and the penta screen. The triple
screen consists of maternal serum AFP, hCG, and uE3 com-
binedwithanaprioririskbasedonmaternalagetoscreenfor
Down syndrome, trisomy 18, and ONTDs. The quad screen
adds DIA, which increases the detection rate for Down syn-
drome (Benn et al. 2003). One laboratory has added invasive
trophoblast antigen (ITA) to the quad screen and named it the
penta screen, although detection rates are not substantially
different from the quad screen (Cole et al. 1999). Second
trimester maternal serum screens are typically performed be-
tween 15w0d-21w6d gestation (Wald et al. 2004). Detection
rates for Down syndrome (75–83 %) and trisomy 18 (60–70 %)
are highest with the quad screen or penta screen (Table 1),
(Wald et al. 2003). Detection rates for ONTDs are the same
for all second trimester screening options (Barkai et al. 1993;
Haddow et al. 1998;Waldetal.2004). Second trimester screens
are helpful for women who first present for prenatal care in their
second trimester, but all second trimester MSS have lower
detection rates compared to screening options that incorporate
first trimester serum analytes. NIPT may represent a viable
alternative for screening with a high detection rate for eligible
patients who present in the second trimester.
A fetal ultrasound in the second trimester may also be used
to screen for chromosome aneuploidy by identifying both true
structural defects and structural variants, which are commonly
referred to as “soft markers” (Table 3). Ultrasound may also
detect isolated structural defects not typically associated with
chromosome aneuploidy. The optimal time to perform an
ultrasou nd to survey fetal anatomy is between 18-20w6d
gestation (ACOG Practice Bulletin No. 101, 2009). The risk
for chromosome aneuploidy is dependent upon not only the
combination of soft markers and/or structural defects seen, but
also the expertise of the provider interpreting the ultrasound
(Nyberg and Souter 2001; Sanders et al. 2002). Chromosome
aneuploidy screening by ultrasound can further be limited by
maternal habitus and fetal position. Approximately 50–70 %
of pregnancies with Down syndrome and 80 % of pregnancies
with trisomy 18 will have anatomical defects and/or markers
identified by the detailed or targeted ultrasound (Nyberg and
Souter 2001). Based on these detection rates, second trimester
anatomy ultrasound alone is not as accurate as MSS or NIPT.
Other ultrasounds, such as growth scans, may also detect
structural anomalies that are associated with chromosome
aneuploidy, but these ultrasounds are not routinely used for
chromosome aneuploidy screening.
Diagnostic Testing Options
Current procedures available for the diagnosis of chromo-
some aneuploidy during pregnancy include: CVS, early
amniocentesis, and amniocentesis (Table 4).
Chorionic Villus Sampling (CVS)
CVS is used for the detection of fetal chromosome aneuploidy
in the first trimester. The accuracy for detection of fetal chro-
mosome abnormalities by CVS is estimated to be 98–99 % due
to the <1 % chance for a mosaic result, defined as some cells
studied showing an abnormality and some cells not showing an
abnormality, and the<1 % chance for maternal cell contami-
nation, defined as studying the mother’s cells instead of the
fetus’ (Ledbetter et al. 1992). CVS may also be used to test for
biochemical abnormalities, single gene conditions, and colla-
gen abnormalities (Pepin et al. 1997; Wapner 2005). CVS
cannot be used to evaluate the risk for ONTDs. The
procedure-related risk of miscarriage is estimated to be approx-
imately 0.5–1%,or1/200–1/100, whether in a singleton or
twin gestation (Canadian Collaborative CVS-Amniocentesis
Clinical T rial Group 1989;CDC,1995; Jackson et al. 1992).
Recent data, however, has shown that the procedure-related
loss rate of CVS may be similar to the rate for mid-trimester
amniocentesis, but this data is only valid in experienced centers
(ACOG Practice Bulletin No. 88, 2007). Of note, there appears
to be an increased risk for limb reduction defects when CVS is
performed prior to 10 weeks gestation (Brambati et al. 1992).
The primary benefit of CVS is that it can be performed at an
earlier gestational age, allowing for earlier decision-making.
Amniocentesis
Amniocentesis is used for the detection of chromosome
aneuploidy in the second and third trimester of pregnancy.
The accuracy for detection of fetal chromosome abnormal-
ities by amniocentesis is estimated to be 99.8–99.9 %
(ACOG Practice Bulletin No. 88, 2007). Amniocentesis
NSGC Practice Guideline 11

may also be used to test for ONTDs, biochemical abnormal-
ities and single gene conditions (CDC, 1995; Winsor et al.
1999). In 1995, the Centers for Disease Control and Preven-
tion released a statement which estimated the procedure-
related risk for miscarriage to be 1/200 or 0.5 % based on
previous studies. Since that time, this number has remained
the universally quoted risk for amniocentesis in the United
States. However, more recent studies actually suggest that
amniocentesis has a much lower risk than the long-accepted
1/200 figure. Data from the First And Second Trimester
Evaluation of Risk for Aneuploidy (FASTER) trial showed
that the miscarriage risk associated with amniocentesis was
approximately 1 in 1600, or less than 0.1 % (Eddleman et al.
2006). In 2007, ACOG released a Practice Bulletin stating
that all women should be offered the option of diagnostic
testing for chromosome aneuploidy, regardless of age, citing
a 1/300 to 1/500 or 0.2–0.3 % risk for miscarriage associat-
ed with amniocente sis based on more recent studies. Many
centers have since adopted this lower, ACOG-e ndorsed
figure (ACOG Practice Bulletin No. 88, 2007). While am-
niocentesis is associated with a lower risk for miscarriage
compared to CVS, one of the primary limitations is the later
gestational age at which the procedure is performed. Waiting
until the third trimester to per form amniocentesis is not
associated with a decreased procedure-related risk; however,
the risk shifts from miscarriage in the second trimester to
preterm delivery in the third trim ester once viability is
reached. Amniocentesis and CVS may be performed in twin
and higher order gestation pregnancies, although the risk for
miscarriage may be increased compared to that associated
with singleton procedures (ACOG Practice Bulletin No. 88).
Early Amniocentesis
Early amniocentesis is available in some centers but is not
typically recommended. It may be performed prior to 15 weeks
of gestation, a nd is associated with an increased risk for
pregnancy loss (2 %), clubfoot (1.3–1.7 %) and fluid leakage
(3.5–4.4 %) compared to routine amniocentesis (<0.1 % for
clubfoot and 1.7 % for leakage), (ACOG Practice Bulletin No.
88, 2007; Canadian Early and Mid-trimester Amniocentesis
Trial, 1998; CDC, 1995; Sundberg et al. 1997).
Screening and Diagnostic Testing Options: Practical
Considerations
Despite numerous potential benefits associated with screening
and testing for chromosome aneuploidy, there are also limita-
tions. Available options may be limited by a number of factors,
including: gestational age of the patient at entry into the health-
care system, state regulations impacting available options, in-
surance coverage and out-of-pocket costs to the patient,
laboratory contracts, availability of laboratory draw sites,
access to certified NT providers, and access to physicians
who perform CVS or amniocentesis. One of the main barriers
faced in screening is insurance coverage, as each private and
public insurance plan has specific requirements for coverage of
screening and diagnostic testing for chromosome aneuploidy.
Additionally, there is often a time lapse between the publication
of guidelines recommending the incorporation of a new test and
routine coverage of that test by insurance companies. These
issues should be considered when assessing a patient’s access to
various prenatal screening and diagnostic testing options.
In addition to external factors that impact testing options,
patient-specific factors also impact decision-making. For
example, patients typically do not view prenatal diagnostic
testing as a routine procedure (Hunt et al. 2005), and may
have conflicting feelings about the possibility of having a
child with a chromosome aneuploidy versus the possibility
of losing a chromosomally normal pregnancy as the result of
a diagnostic procedure (Kupperman et al. 2000). It is up to
the healthcare provider to explore these feelings and discuss
factors that influence decision-making, such as family, so-
cial, and personal history, maternal age, and possible out-
comes in order t o obtain informed consent (Centers for
Disease Control and Prevention 1995). Current practice is
moving away from a maternal age-based risk stratification
for offering diagnostic testing and moving toward custom-
ized risk assessment through the use of the various screen-
ing methods discussed above (ACOG Practice Bulletin
No.88, 2007; Eddleman et al. 2006).
The purpose of the following recommendations is to
assist physicians and allied health professionals in identify-
ing appropriate screening and diagnostic testing options for
chromosome aneuploidy for their patients. Patients may
have differing levels of in ter est in the available options
based on how they feel they might utilize the information.
Recommendations
The information presented above, along with the data sum-
marized in Fig. 1, and Tables 1, 2, 3 and 4 supports the
following recommendations:
Recommendations for all patients
& Providers should offer the options of maternal serum
screening (MSS) and diagnostic testing for chromosome
aneuploidy to every patient.
– Providers should engage in a discussion with their
patients about the benefits, limitations, and risks
of MSS and diagnostic testing so that patients may
make informed and autonomous decisions.
– If the provider feels a patient would benefit from
additional discussion prior to making a decision, a
12 Wilson et al.

referral to a genetic counselor or other qualified
provider may be appropriate.
– Documentation of the patient’s decision to elect
or to decline screeningandtestingshouldbe
made in the patient’s medical record.
– Providers should be aware of factors that may
impact the options available to their patients, such
as the patient’s gestational age, insurance cover-
age and access to services and providers.
& An ultrasound to assess the fetal anatomy is suggested at
approximately 18w0d-20w0d gestation for all patients
regardless of whethe r or not they choose to have screen-
ing or diagnostic testing.
Recommendations for low risk patients less than 14 weeks
of gestation:
& For patients who may consider CVS or amniocentesis,
stepwise sequential screening or combined first trimes-
ter screening should be considered because:
– Both are tailored to fit t he needs of patients
who desire early detection of chromosome
aneuploidy but wish to employ a screening meth-
od prior to making a decision about diagnostic
testing.
– Both allow for the option of CVS in higher risk
pregnancies while deferring testing of lower risk
pregnancies to the second trimester without caus-
ing increased anxiety.
– Of the screening options that provide risk infor-
mat ion in the first trimester, stepwise sequential
screening has the highest detection rates for Down
syndrome and trisomy 18.
& If CVS is not an option, integrated screening may be
considered in order to maximize detection rates.
& If a patient completes combined first trimester screening,
a separate second trimester MSS for chromosom e aneu-
ploidy is NOT indicated. Screening for chromosome
aneuploidy in the second trimester in patients who
present prior to 14 weeks should ONLY be performed
as a part of integrated, serum integrated, stepwise
sequential, or contingency screening. Independent
screening in first and second trimesters increases the
false positive rate of screening.
& Patients who have an increased NT (≥ 95th% or≥
3.0mm) should be offered diagnostic testing by ei-
ther CVS or amniocente sis. A referral for a fetal
echocardiogram should also be considered if the
NT ≥3.5mm.
& Early amniocentesis (pri or to 15 weeks of gestation) is
not recommended due to the increased risks for preg-
nancy loss, clubfoot, and fluid leakage. CVS should be
offered as the diagnostic testing option for chromosome
aneuploidy in the first trimester.
Recommendations for low risk patients after 14 weeks of
gestation:
& Patients who desire MSS but did not have MSS in the
first trimester should be offered a quad or penta screen
rather than a triple screen due to the increased detection
rates.
& Amniocentesis should be offered as the diagnostic test-
ing option for chromosome aneuploidy for patients after
15 weeks of gestation.
Recommendations for patients at increased risk for
chromosome aneuploidy
& Patients who desire screening information may be of-
fered NIPT due to the high detection rates and low false
positive rates. NIPT should only be offered in the con-
text of informed consent, edu cation, and counseling by a
qualified provider, such as a genetic counselor. Standard
confirmatory diagnostic testing should be offered as
follow-up to positive NIPT results. High risk patients
who decline NIPT but remain interested in screening
should be made aware of alternate screening options as
appropriate based on gestational age and screening
availability.
& If the patient presents prior to 14 weeks gestation, CVS
and amniocentesis should both be offered as diagnostic
testing options for chromosome aneuploidy.
& If the patient presents after 14 weeks gestation, amnio-
centesis should be offered as the diagnostic testing op-
tion for chromosome aneuploidy.
Summary
This practice guideline provides a summary of screening
and diagnostic testing options for chromosome aneuploi-
dy and gives realistic recommendations on how to em-
ploy these options. A decision tree and com parison
tables are presented for providers to select the screening
or diagnostic test which best suits their patient’s needs.
Specific recommendations are given for certain clinical
circumstances. However, these options are dependent on
logistical factors such as t iming of entry into healthcare,
insurance coverage, overall cost, and screening/testing
availability. Patients will make decisions regarding these
options based not only on the facts and the data, but
also based on personal feelings, past experiences, and
current perceptions. A referral to a genetic counselor or
other qualified provider may be appropriate if a patient
may benefit from additional discussion prior to making
NSGC Practice Guideline 13
