REVIEW ARTICLE
Telehealth in the rehabilitation of female pelvic floor dysfunction:
a systematic literature review
Kyannie Risame Ueda da Mata
1
& Rafaela Cristina Monica Costa
1
& Ébe dos Santos Monteiro Carbone
1,2
&
Márcia Maria Gimenez
1,2
& Maria Augusta Tezelli Bortolini
2
& Rodrigo Aquino Castro
2
& Fátima Faní Fitz
1,2
Received: 31 July 2020 /Accepted: 23 October 2020
#
The International Urogynecological Association 2020
Abstract
Introduction and hypothesis The pandemic caused by coronavirus disease 2019 (COVID-19) increased the awareness and
efforts to provide care from distance using information technologies. We reviewed the literature about the practice and effec-
tiveness of the rehabilitation of the female pelvic floor dysfunction via telehealth regarding symptomatology and quality of life
and function of pelvic floor muscles (PFM).
Methods A bibliographic review was carried out in May 2020 in the databases: Embase, Medline/PubMed, LILACS and PEDro.
A total of 705 articles were reviewed after the removal of duplicates. The methodological quality of the articles was evaluated by
the PEDro scale. Two authors performed data extraction into a standardized spreadsheet.
Results Four studies were included, two being randomized controlled trials. Among the RCTs, only one compared telehealth
with face-to-face treatment; the second one compared telehealth with postal treatment. The other two studies are follow-up and
cost analysis reports on telehealth versus postal evaluation. Data showed that women who received the intervention remotely
presented significant improvement in their symptoms, such as reducing the number of incontinence episodes and voiding
frequency, improving PFM strength and improving quality of life compared to women who had the face-to-face treatment.
Conclusions Telehealth promoted a significant improvement in urinary symptoms, PFM function and quality of life. Telehealth is
still emerging, and more studies are needed to draw more conclusions. The recommendations of the governmental authorities,
physical therapy councils and corresponding associations of each country also need to be considered.
Keywords Telemedicine
.
Telemotoring
.
Pelvic floor
.
Urinary incontinence
.
Women’shealth
Introduction
Telehealth involves health care services, support and informa-
tion provided remotely via digital communication and de-
vices. It intends to facilitate effective delivery of health ser-
vices such as physical therapy by improving access to care and
information and managing health care resources [1]. Other
terms such as telemedic ine, telemonitoring, tele-education
and tele-assistance describe digital practice [2]. Due to the
pandemic caused by coronavirus disease 2019 (COVID-19),
health associations worldwide have released recommenda-
tions about care from distance using tools of communication
and information technologies [3–5].
In clinical practice, however, it is still unclear how the
professionals can perform rehabilitation of female pelvic floor
dysfunction via telehealth.
Before starting a pelvic floor muscle (PFM) training pro-
gram, one must ensu re that the patients are able to perform a
correct PFM contraction [6]. More than 30% of women are not
able to voluntarily contract the PFM at their first consultation
even with individual instruction verbally and by using digital
manual therapy [7, 8]. The success rate varies from 60% to 75%
when the PFM exercises are performed in the outpatient setting
[9, 10]. The literature has shown that home PFM training
(PFMT) provides equal benefit to outpatient PFMT in reducing
Supplementary Information The online version contains
supplementary material available at https://doi.org/10.1007/s00192-020-
04588-8.
* Fátima Faní Fitz
fanifitz@yahoo.com.br
1
Centro Universitário São Camilo, São Paulo, SP, Brazil
2
Department of Gynecology, Universidade Federal de São Paulo, Rua
Napoleão de Barros, 608 - Vila Clementino, São Paulo, SP CED
04024-002, Brazil
International Urogynecology Journal
https://doi.org/10.1007/s00192-020-04588-8

urinary symptoms when the patients attend some outpatient
sessions to monitor their exercises during their treatment [11,
12]. So, the question in telehealth is: How can we perform
rehabilitation of the pelvic floor in women in order to overcome
the issues of not using manual therapy in the process of pelvic
floor evaluation and teaching of PFM contraction?
Due to the COVID-19 pandemic, adequate patient care is
urgently needed. So, alternatives in this dynamic clinical sit-
uation include systematic review as a way to connect evidence
and practice and to guide clinical care [13]. Therefore, the
purpose of the present study was to review telehealth in female
pelvic floor dysfunction rehabilitation. The outcome of inter-
est was the methodology by which the digital practice can be
performed. Secondarily, pelvic floor symptoms, quality of life
and function of the PFM were assessed.
Methods
Protocol and registration
This systematic review was developed following the PRISMA
guidelines. The systematic review protocol was registered in
the PROSPERO database under number CRD42020200457.
Eligibility criteria and study selection
Studies were eligible for inclusion if they were randomized
controlled trials and clinical trials that used telehealth in reha-
bilitation of female pelvic floor dysfunction. For this review,
digital practice was regarded as health care services, support
and information provided remotely via digital communication
as a form of intervention. We excluded studies that aimed only
to investigate new technologies such as mobile applications
and digital devices for home treatment with no comparator.
Information sources and search
The literature search was performed on May 2020 and includ-
ed studies from inception with no language restriction. The
consulted datab ases were: Embase, Medline/PubMed,
LILACS and PEDro (Physiotherapy Evidence Database).
The keywords u sed were: Telerehabi litation; Internet;
Videoconferencing; Tele; Continence; Women’sHealth;
Pelvic Floor; Telehealth; Urinary Incontinence ; Muscle
Dysfunction; Sexual Dysfunction; Pelvic Pain; Fecal
Incontinence; Pelvic Organ Prolapse. The search strategies
are described in the supplemental material (Supplement 1).
Screening and data extraction
A data search was performed by the authors (K.R.U.M. and
R.C.M.C.). A third author (F.F.F.) was consulted for a consensus
if discrepancies occurred. A standardized data extraction form
was used to collect the following data: authors, year of public a-
tion, journal, country of o rigin, sample, age (years), obje ctives,
outcome measure and results/conclusio ns. Data extraction was
performed by two independent raters (E.S.M.C. and M.M.G.).
Outcomes
The primary outcome was to investigate the telehealth meth-
odologies used by health professionals for PFM rehabilitation.
Secondarily, we investigated the effectiveness of telehealth in
PFM rehabilitation considering pelvic floor symptoms and
quality of life as well as PFM function in women with pelvic
floor dysfunctions.
Risk of bias assessment and analysis
The methodological q uality of the trials was assessed using the
PEDro scale (values of 0–10), with scores extracted from the
PEDro database [14]. The assessment of the quality of trials
was performed by two independent raters (M.A.T.B. and
R.A.C.), and disagreements were resolved by a third rater
(F.F.F.). Methodological quality was not an in clusion criterion.
As data were extracted and described, heterogeneity between
the outcomes did not allow poolin g data and performing sub-
group analysis or metanalysis. Results were displayed in tables in
a synthesized format. The description followed a narrative review
format.
Results
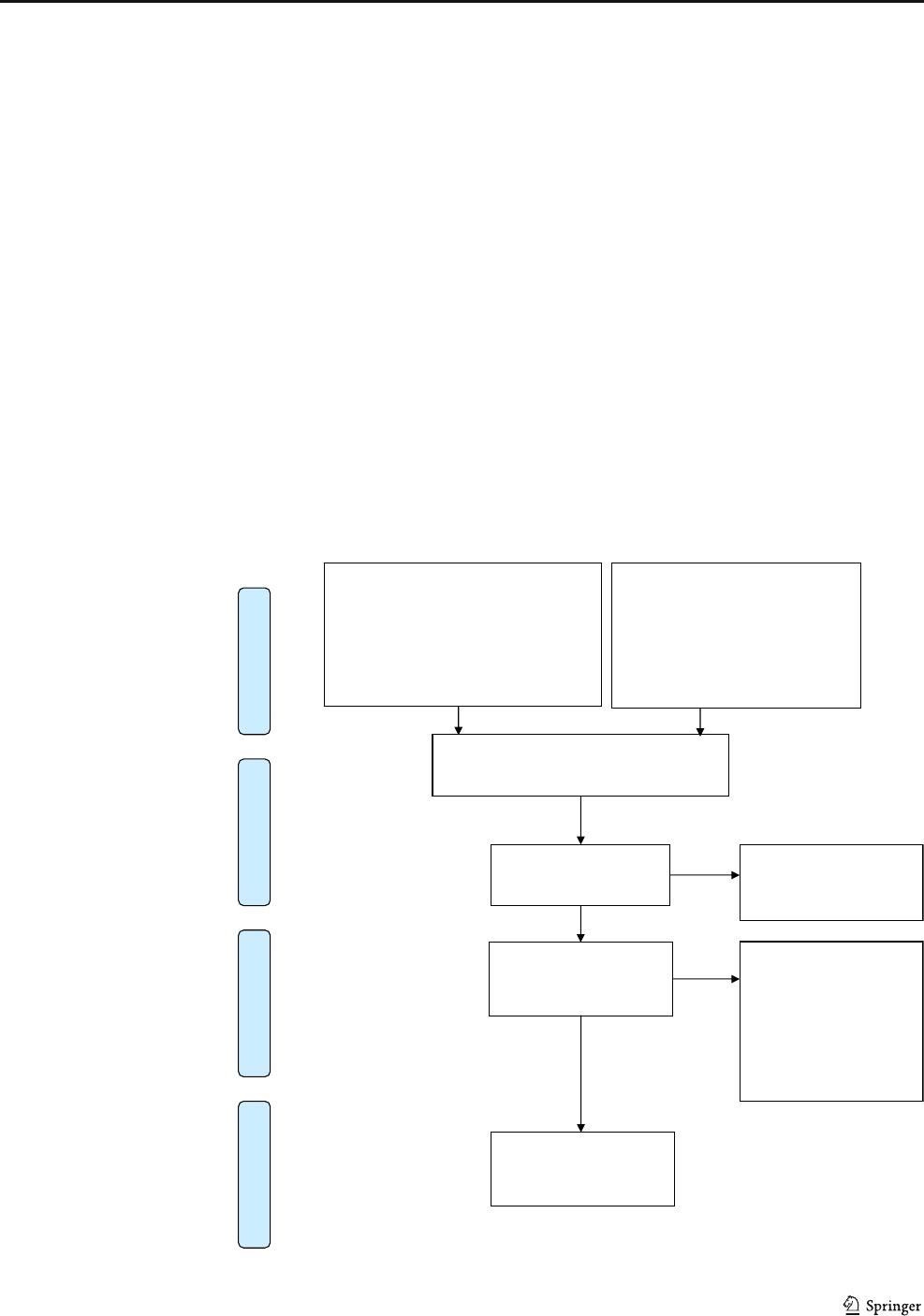
The first electronic database search resulted in a total of 705
articles after the removal of duplicates. As shown in Fig. 1,
eight articles were selected as potentially eligible on the basis
of their title and abstract, and four were excluded from analy-
sis after reading in full [15–18]. A total of four articles were
included in this review [19–21].
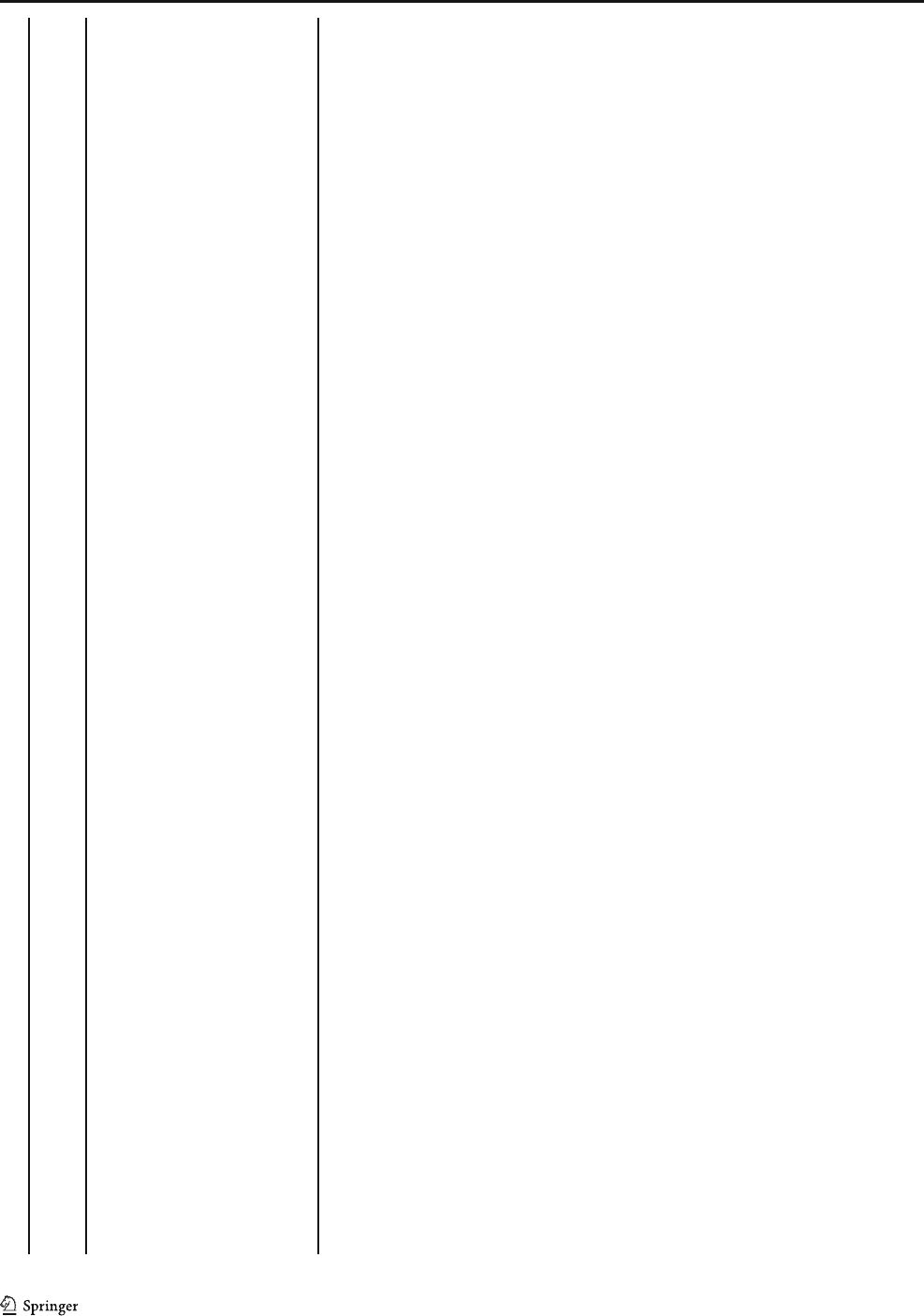
The methodological quality assessment by the PEDro scale
revealed a median score of 5 (range 4–6) (Table 1). Random
allocation, adequate follow-up, between-group comparisons
and point estimates and variability were included in all trials.
Concealed allocation, blind subjects, blind therapists and
blind assessors were not included in all trials. Comparability
at baseline was included in three trials [19, 20, 22]. Intention-
to-treat analysis was reported in two publications [19, 20].
The articles included in this review investigated telehealth
in the treatment of stress urinary incontinence (SUI) and urge
urinary incontinence. Only two studies were original random-
ized controlled trials [19, 22]. The other two publications were
a follow-up [20] and cost analysis [21] of the study developed
by Sjostrom et al. [19]. The details of the studies are described
in the Table 2.
Int Urogynecol J
Telehealth—How is it performed?
The studies included in this review investigated the internet-
based program versus postal program [19–21] and conven-
tional treatment (face-to-face intervention) [22].
In Sjostrom et al.’s study, the patients were recruited via an
open access website. Invitations to the study were published on
national websites for medical advice and as advertisements in
daily newspapers. To confirm the clinical diagnosis of SUI, all
participants were interviewed via telephone. The contact with
patients during the intervention was asynchronous, with
encrypted e-mail, requiring a separate login from b oth partici-
pants and therapists. The therapist gave the participant login
codes for two levels at a time, with instructions to maintain
training at each level for at least 1 week. The participants com-
pleted a self-evaluated test and reported a training diary to the
therapist weekly. New login codes were given with the passing
of every other test. The participants could contact their therapist
at any time for support or questions. Response from the thera-
pist was promised within 3 working day s, and sep arate
technical support was offered through encrypted e-mail contact
with the website manager. The program was built on a secure
platform, using a two-factor authentication and Secure Sockets
Layer (SSL) to provide communication security over the inter-
net. All parts of the program could be downloaded for printing
[19]. In this study, the authors compared telehealth with an
exercise program sent by post. The patients received a print
version containing information about the program, followed
by instructions for PFM training. The participants in this group
had no contact with the urotherapists [19].
Hui et al. performed the PFM program via videoconferenc-
ing. The sessions were carried out in a private and quiet room
in the community center. Subjects were reassured that they
were only sharing the progress of their incontinence symp-
toms with other participants in the session. The nurse special-
ist provided behavioral training to the group via videoconfer-
encing with the support of a research assistant at the patients’
end. The patients shared their experiences with the nurse and
were encouraged to adhere to behavioral training and PFM
exercises [22].
Records idenfied through database
searching
Medline/PubMed= 668
LILACS= 17
PEDro= 28
Total aer removing duplicates (n= 703)
Screening
Included
Eligibility
Idenficaon
Addional records idenfied through
other sources
(n= 0)
Records aer duplicates removed
(n= 705)
Records screened
(n= 8)
Records excluded aer
reading tle and abstract
(n= 697)
Full-text arcles assessed
for eligibility
(n= 8)
Full-text arcles excluded,
with reasons (n= 4)
The studies invesgated
the mobile device
(smartphone) to treat
pelvic floor dysfuncons
15-
18
Arcles included in this
review
(n= 4)
Fig. 1 PRISMA flow diagram for
the selected studies
Int Urogynecol J
Effects of telehealth on PFM function, urinary
symptoms and quality of life
Three articles from the same Swe dish group showed the
findings of a program for SUI treatment via the internet
versus by post on the same cohort of 250 women [19–21].
One publication presented the results on urinary symptoms,
cure and quality of life after 4 months of treatment using
questionnaires sent by post mail [19]; another publication
reported the same outcomes at 1- and 2-year follow-up
[20]; the last article addressed the costs of the two interven-
tions [21].
Sjostrom et al. [19] described significant improve-
ments in both i nterventions (internet and postal groups)
after ITT analysis, but there were no significant differ-
ences between groups in urinary symptoms and
condition-specific quality of life after 4-month treatment.
Regarding subjective cure, more participants in the i nter-
net group reported being much or very much improved
( p = 0.01), had reduced use of incontinence pads (p =
0.02) and were satisfied with the treatment program
(p < 0.001) compared to t he postal group. Quality of life
improved in the internet group (p = 0.001), but not in the
postal group (p = 0.13). Overall, 69.8% (120/172) o f the
participants reported absence or reduced number of UI
episodes by > 50% [19]. Loss to follow- up rate was 12% .
The authors report 32% loss of participants at 1-year and
38% at 2- year follow-up assessments. Highly significant
(p < 0.001) improvements were observed f or symptoms
and condition-specific quality of life after 1 and 2 years,
respectively, for both internet and postal interventions, with-
out significant differences between groups. The proportions
of participants perceiving they were much or very much
improved were similar in both intervention groups after
1year(p = 0.82), but after 2 years significantly more partic-
ipants in the internet group reported this degree of improve-
ment (p = 0.03). At 1 year after treatment, 69.8% of partici-
pants in the internet group and 60.5% of participants in the
postal group reported that they were still satisfied with the
treatment result. After 2 years, the proportions were 64.9%
and 58.2%, respectively [20].
The authors measured quality of life w ith the ICIQ-
LUTSqol condition-specific questionnaire and calculated
the quality-adjusted life-years (QALYs) gained to estimate
the cost-effectiveness. Compared to the postal program, the
extra cost per QALY for the internet-based program ranged
from 200€ to 7.253€, indicating greater QALY gains at sim-
ilar or slightly higher costs. Compared to no treatment, the
extra cost per QALY for the internet-based program ranged
from 10.022€ to 38.921€, indicating greater QALY gains at
higher but probably acceptable costs. The authors concluded
that an internet-based treatment for SUI is a new, cost-
effective treatment alternative [21].
Table 1 PEDro scale for the methodological quality assessment
Study Eligibility 1. Random
allocation
2. Concealed
allocation
3. Baseline
comparability
4. Blind
subjects
5. Blind
therapists
6. Blind
assessors
7. Adequate
follow-up
8. Intention-to-
treat analysis
9. Between-group
comparisons
10. Point estimates
and variability
Total
Score
Sjostrom
et al., 2013
[19]
++ – + –– – ++ + + 6
Sjostrom
et al., 2015
[20]
++ – + –– – ++ + + 6
Sjostrom
et al.,2015
[21]
++ –– –––+ – ++ 4
Hui et al., 2006
[22]
++ – + –– – + – ++ 5
Eligibility criteron item does not contribute to the total score; + criterion is clearly satisfied; − criterion is not satisfied
Int Urogynecol J

Table 2 Details of the included randomized controlled trials
Reference Study design/
period/country
Participant characteristics, sample size
(N), duration of symptoms
Interventions Outcomes (measures) and time points;
results; conclusion
Sjostrom
et al.,
2013
[19]
RCT/December
2009 to April
2011/
Sweden
Age = 18–70 years
N =250
Duration of symptoms = SUI ≥ 1
time/week
Inclusion
criteria = community-dwelling
women with SUI at least once a
week that matched with age. Ability
to read and write Swedish and sccess
to computer with internet
connection
Exclusion criteria = pregnancy,
previous incontinence surgery,
known malignancy in lower
abdomen, difficulties passing urine,
macroscopic hematuria,
intermenstrual bleedings, severe
psychiatric diagnosis, and
neurological disease affecting
sensibility in legs or lower abdomen
Dropout rate = 32.4%
Internet-based group = information on
SUI and associated lifestyle factors;
PFMT; training reports (frequency,
time spent). This group received
asynchronous, individually tailored
e-mail support from a urotherapist
during the treatment period
Postal group = information on SUI and
associated lifestyle factors; PFMT;
training reports (frequency, time
spent). Participants in this group had
no contact with the urotherapists
Follow-up: 4 months via self-assessed
postal questionnaires
Primary outcomes = International
Consultation on Incontinence
Questionnaire Short Form (ICIQ-UI
SF); International Consultation on
Incontinence Questionnaire Lower
Urinary Tract Symptoms Quality of
Life (ICIQ-LUTSQoL)
Secondary outcomes = Patient Global
Impression of Improvement (PGI-I);
urinary incontinence aids; patient
satisfaction; EuroQol 5D-Visual
Analogue Scale (EQ5D-VAS); in-
continence episode frequency (IEF)
Results = intention-to-treat analysis
showed high significance with both
interventions, but there were no
significant differences between
groups in primary outcomes. 40.9%
of internet group perceived they
were much or very much improved;
59.5% reported reduced usage of
incontinence aids; 84.8% were
satisfied with the treatment program
vs. 26.5%; 41.4% and 62.9%,
respectively, of postal group
Conclusion = Concerning primary
outcomes, treatment effects were
similar between groups whereas for
secondary outcomes the
internet-based treatment was more
effective. Internet-based treatment
for SUI is a new, promising treat-
ment alternative
Sjostrom
et al.,
2015
[20]
Follow-up was performed after 1 and
2 years via self-assessed postal
questionnaires
There was no face-to-face contact with
the participants at any time
Results = Within both treatment
groups, there were highly significant
improvements in the primary
outcomes, ICIQ-UI SF and
ICIQ-LUTSqol, after 1 and 2 years
compared with the baseline. The
difference between the groups was
not significant after 1 year. After
2 years, significantly more partici-
pants in the internet group rated their
leakage as much or very much im-
proved than was the case in the
postal group. Health-specific QoL
did not improve significantly in any
of the treatment groups after 1 year.
However, after 2 years there was
significant improvement within the
internet group, but not within the
postal group. The differences be-
tween the groups were not signifi-
cant
Conclusion = Non-face-to-face
treatment of SUI with PFMT
provides significant and clinically
relevant improvements in symptoms
and condition-specific QoL at 1 and
2 years after treatment
Int Urogynecol J

Table 2 (continued)
Reference Study design/
period/country
Participant characteristics, sample size
(N), duration of symptoms
Interventions Outcomes (measures) and time points;
results; conclusion
Sjostrom
et al.,
2015
[21]
Included all relevant costs accrued
during the first year, regardless of
who paid for them. Prices per unit
were multiplied by the amount
consumed and added up to a sum
representing the total societal cost.
All costs are given in euros at the
2010 mid-year level
Follow-up = 1 year
Outcomes = incremental cost
effectiveness ratio (ICER);
International Consultation on
Incontinence Questionnaire Short
Form (ICIQ-UI SF); International
Consultation on Incontinence
Questionnaire Lower Urinary Tract
Symptoms Quality of Life
(ICIQ-LUTSQoL); quality-adjusted
life-years (QALYs).
Results = compared to the postal
program, the extra cost per QALY
for the internet-based program
ranged from 200€ to 7253€,indi-
cating greater QALY gains at simi-
lar or slightly higher costs.
Compared to no treatment, the extra
cost per QALY for the
internet-based program ranged from
10,022€ to 38,921€, indicating
greater QALY gains at higher, but
probably acceptable costs
Conclusion = an internet-based treat-
ment for SUI is a new, cost-effective
treatment alternative
Hui et al.,
2006
[22]
RCT/not
reported/
China
Age = 60 years or over
N =58
Inclusion
criteria = community-dwelling older
women aged 60 years or over, with
symptoms of urge or SUI, and with
one or more incontinence episodes
in a week
Exclusion criteria = active urinary tract
infection, a post-void residual vol-
ume by bladder ultrasound >
150 ml, third-degree uterine pro-
lapse and those already receiving
treatment for their urinary symptoms
Telemedicine continence group
(TCP) = 8-week intervention period
with one session per week by
videoconferencing
Continence service (CS) = 8-week
intervention period with one session
per week face to face
At baseline, both groups were assessed
face to face for pelvic floor muscle
strength, instrumental biofeedback
and verbal feedback by vaginal
palpation.
During the intervention period, all
components of behavioral training
given to either intervention group
were identical, with one exception in
the TCP group, where it was not
possible for the nurse specialist to
give feedback on pelvic floor
contraction during follow-up, as
digital assessment could not be
performed
Outcomes = perception of the severity
of incontinence symptoms and level
of satisfaction (0 = none, 1 = mild,
2 = moderate, 3 = severe); 3-day
voiding diary (number of inconti-
nent episodes, voiding frequency
and voided volume); pelvic floor
muscle strength by digital assess-
ment [Oxford Scale (0 = none, 1 =
flicker, 2 = weak, 3 = moderate, 4 =
good, 5 = strong)]; satisfaction with
the TCP on a 6-point Likert scale
(0 = highly dissatisfied to 5 = highly
satisfied).
Results = participants in both treatment
groups experienced significant
improvement in their symptoms
with a reduction in the number of
daily incontinence episodes and
voiding frequency, while the
volume of urine at each micturition
increased. Pelvic floor muscle
strength also improved. There were
no significant differences in
outcomes between the two groups
Conclusion = results suggested that
videoconferencing is as effective as
conventional methods in the
management of urinary incontinence
PFMT pelvic floor muscle training,
SUI stress urinary incontinence, ICIQ-UI SF International Consultation on Incontinence Questionnaire Short Form,
ICIQ-LUTSqol International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms Quality of Life, PGI-I Patient Global
Impression of Improvement, EQ5D-VAS EuroQol 5D-Visual Analogue Scale, IEF incontinence episode frequency, ICER incremental cost effectiveness
ratio, QALYs quality-adjusted life-years, TCP telemedicine continence group, CS continence service
Int Urogynecol J

Hui et al. compared telemedicine with conventional outpa-
tient sessions (face to face) in 58 community-dwelling older
women with urgency or SUI. There were no significant dif-
ferences in outcomes between the two groups. Participants in
both treatment groups experienced significant improvement in
their symptoms, namely, reduction in the number of daily
incontinence episodes (p < 0.001) and voiding frequency (p
< 0.001), while the volume of urine at each micturition in-
creased (p < 0.005). PFM strength as measured by the
Oxford Scale also improved (p <0.005)[22].
Discussion
Telehealth is an alternative way to provide rehabilitation ser-
vices. Technological advances prove to be a facilitator in the
communication between the health professional and the pa-
tient especially in remote locations, presenting great potential
as a substitute or as a complement to current therapies [23].
Digital practice is not a modality used in all countries and
depends on the local regulations.
The main question is how to use digital technology in the
clinical practice of PFM rehabilitation. In this review we gath-
ered data from two controlled trials that addressed
teleconsultation and telemonitoring in the rehabilitation of
PFM for the treatment of urinary disorders [19–22].
Sjostrom et al. used a PFMT program via the internet com-
pared to a postal program. For the authors a standardized face-
to-face treatment or care as usual would have been an option
to compare the internet modality, but they wanted the treat-
ment program to be accessible to women from all over the
country, even from remote areas or from areas with inadequate
staffing [19]. Both modalities were shown to be beneficial
treatments after 4-month intervention [19] and at 1 and 2 years
after treatment [20]; thus, management of SUI without face-
to-face contact is possible and may increase access to care.
The authors also found the internet-based treatment is an ef-
fective new, promising, alternative treatment [19, 20].
Before starting a PFM training program, one has to ensure
that the patients are able to perform a correct PFM contraction
[6]. In the study developed by Sjostrom et al., all the interven-
tions were made without PFM evaluation. The authors did not
explain how the patients were directed to perform the PFM
contraction, but they acknowledged that the ability to under-
stand written instructions, carry them out and adequately use a
computer were prerequisites to succeed with a treatment com-
pleted on one’s own in the internet group [19].
On the other hand, Hui et al. assessed the PFM strength
face to face with biofeedback (BF) and vaginal palpation at
baseline in both groups (telemedicine continence group and
conventional group) in their study [22]. The literature suggests
the utilization of sensor technologies to sample and quantify
movement in telehealth [24]. BF equipment uses sensors to
measure PFM contraction and maybe can be used in
telehealth. There is no consensus in the literature on whether
BF can be used to promote awareness of the PFM. Some
authors have tried to make patients more aware of muscle
function [25]. To date, there are no studies investigating the
effect of BF in a population that is not able to contract the
PFM. In others’ opinions, it is difficult to understand how the
BF machine can teach the patient how to contract the PFM
without verbal instruction and manual techniques explained
by the therapist [26].
Conservative treatment depends heavily on physical touch,
and therapists rely on the objective measurement of physical
performance to inform diagnosis and intervention [24]. With
this, therapies that do not typically involve hands-on assess-
ment are best suited to digital practice. Even though in PFM
rehabilitation it is difficult to adapt the practice to provide
services via information and communication technologies, as
hands-on assessment and treatment are typically involved, it
seems that it is feasible to teach the correct PFM contraction
technique with verbal instructions and drawings of the anato-
my of the pelvic floor and to help the patients understand the
action of the PFM, describing the contraction as a lift starting
with closure of the doors (squeeze) and from there the elevator
is moving upstairs (lift) [6].
The virtual environment can be displayed to the patient via
computer screen, or fully immersive environments are possi-
ble with the use of head-mounted visual displays and feedback
devices [24]. Sjostron et al. used a program developed on a
secure platform with two-factor authentication [19]. Hui et al.
used videoconferencing, and participants shared their experi-
ences with the group members. The only request was that the
patients remain in a private and silent room [22]. A private
environment, with the use of headphones so that other profes-
sionals and/or family members do not have access to the ses-
sion, should be recommended. The risk of leakage of infor-
mation related to digital care always exists and must be shared
with patients, and, whenever possible, safer professional plat-
forms should be used [27].
The patient’s knowledge and ability related to the virtual
environment must be considered. Some patients considered
the double logins complicated in the study of Sjostrom et al.
[19]. Therefore, it is recommended that service providers en-
sure that technical requirements are met, provide access to
technical support and provide training to all users [23]. The
lack of ability and knowledge related to handling technologies
are the disadvantages of telerehabilitation [28].
The literature reports that the savings of transportation
costs and of the health care system’s and patient’s time, the
continuity of patient care that can be achieved through the
remote provision and the heightened abil ity to control the
timing, intensity and sequencing of the intervention are advan-
tages of telerehabilitation [24]. The questions are whether the
professionals are prepared to implement digital practice and
Int Urogynecol J

how they can offer telerehabilitation services, especially in the
area of pelvic floor dysfunction rehabilitation. This type of
service is a growing field, adopted within the COVID-19 pan-
demic, and has the potential to reduce costs, increase the over-
all accessibility of modern health care systems and open new
perspectives for rehabilitation in pelvic floor dysfunctions [2,
29]. A guide with specific issues involving digital practice in
physical therapy needs to developed. And the governmental
authorities, physical therapy councils and corresponding asso-
ciations of each country should be involved.
The limitations of this study include the scarcity of litera-
ture related to telehealth, especially compared to conventional
treatment (face to face). The study performed by Hui et al. was
the only one that compared telehealth with conventional treat-
ment. The authors concluded that telehealth is as effective as
conventional treatment for urinary incontinence [22]. The lit-
erature reports on telehealth and conventional treatment in
other fields of medicine that require conservative therapy.
As with all fields and interventions, effective telehealth re-
quires that therapists understand the essential components of
their treatments and ensure that they are carefully included in
care [28, 29]. Thus, because of the specificity of each field, it
is not possible to discuss the results found by Hui et al. with
further scientific depth. Another limitation is the fact that the
review was carried out in a short period, limiting the search in
the gray literature, and the article was produced quickly so that
it could be useful to professionals and patients.
Conclusion
The literature on digital practice in the treatment of pelvic
floor dysfunction is scarce. Only two original studies have
investigated telehealth in SU I treatment, and one of them
was without a face-to-face group. Telehealth promoted a sig-
nificant improvement in urinary symptoms, PFM function and
quality of life. The results of the studies showed that internet-
based treatment is a promising treatment alternative.
However, this type of assistance still needs to be studied to
verify its real benefits in the treatment of pelvic floor dysfunc-
tions, since further clarification is needed on how to perform
it. The recommendations of governmental authorities, physi-
cal therapy councils and corresponding associations of each
country also need to be considered.
Compliance with ethical standards
Conflict of interest The authors declare no conflicts of interest.
Abbreviations COVID-19, Coronavirus Disease 2019; PFM, Pelvic
floor muscle; PFMT, Pelvic floor muscle training; PEDro,
Physiotherapy Evidence Database; SUI, Stress urinary incontinence
Appendix
PEDro: Telerehabiltation AND Continence and women’s
health; Tele AND Continence and women’s health; Video
conferecing AND Continence and women’s health; Internet
AND Continence and women’shealth.
LILACS: Telerehabilitation AND Pelvic Floor;
Telerehabilitation AND Telehealth AND Women’s Health;
Videoconferencing AND Pelvic Floor; videoconfe rencing
AND Urinary Incontinence (tw:(Pelvic Prolapse)) AND
(tw:(telerehabilitation)); (tw:(telerehabilitation)) AND
(tw:(telehealth)) AND (tw:(women’ s health)) AND
(tw:(Pelvic Prolapse)); (tw:(women’s health)) AND
(tw:(Pelvic Prolapse)) AND (tw:(Video Virtual));
(tw:(Videoconferencing)) AND (tw:(Pelvic Prolapse));
(tw:(Videoconferencing)) AND (tw:(fecal incontinence));
(tw:(Video Virtual)) AND (tw:(fecal incontinence));
(tw:(telerehabilitation)) AND (tw:(women’shealth))AND
(tw:(fecal incontinence)).
PubMed: ((Internet) AND Continence) AND Women’s
Health; (Tele) AND Pelvic Floor; (Internet) AND Pelvic Floor;
(((Telerehabilitations) OR (Tele-rehabilitation) OR (Tele rehabil-
itation) OR (Tele-rehabilitations) OR (Remote Rehabilitation)
OR (Rehabilitation, Remote) OR (Rehabilitations, Remote) OR
(Remote Rehabilitations) OR (Virtual Rehabilitation) OR
(Rehabilitation, Virtual) OR (Rehabilitations, Virtual) OR
(Virtual Rehabilitations) OR)) AND Pelvic Floor; (Video
Conferencing) AND Pelvic Floor; (Video Conferencing) AND
Pelvic Floor; (((((Telehealth) AND Women ’s Health)) AND
((Telerehabili tation) OR (Tele-rehabili tation) OR (Tele rehabi li-
tation) OR (Tele-rehabilitations) OR (Remote rehabilitation) OR
(Rehabilitation, remote) OR (Rehabil itation s, remote) OR
(Remote rehabilitations) OR (Virtual rehabilitation) OR
(Rehabilitation, virtual) OR (Rehabilitations, virtual ) OR
(Virtual rehabilitations)))) AND ((Video conferencin g) AND
Pelvic floor muscle dysfunction); (((((Telehealth) AND
Women’s health)) AND ((telerehabi litation) OR (t ele-
rehabilitation) OR (tele rehabilitation) OR (tele-rehabilitations)
OR (remote rehabilitation) OR (rehabilitation, remote) OR (reha-
bilitations, remote) OR (remote rehabilitations) OR (virtual reha-
bilitation) OR (rehabilitation, virtual) OR (rehabilitations, virtual)
OR (virtual rehabilitations)))) AND ((vide o conferencing) AND
pelvic floor muscle dysfunction); (((teleheal th) AND women’s
health)) AND ((telerehabilitation) OR (tele-rehabilitation) OR
(tele rehabilitation) OR (tele-rehabilitations) OR (remote rehabil-
itation) OR (rehabilitation, remote) OR (rehabilitations, remote)
OR (remote rehabilitations) OR (virtual rehabilita tion) OR (reha-
bilitation, virtual) OR (rehabilitations, virtual) OR (virtual reha-
bilitations)); (telehealth) AND women’ s health;
(((((telerehabilitation) OR (tele-rehabilitation) OR (tele rehabili-
tation) OR (tele-rehabilitations) OR (remote rehabilitation) OR
(rehabilitation, remote) OR (rehabilitations, remote) OR (remote
rehabilitations) OR (virtual rehabilitation) OR (rehabilitation,
Int Urogynecol J

virtual) OR (rehabilitations, virtual) OR (virtual rehabilitations)))
AND Women’s health)) AND telehealth; (video conferencing)
AND pelvic floor muscle dysfunction; (video conferencing)
AND pelvic floor muscle dysfunction; ((((Telerehabilitations)
OR (Tele-rehabilitation) OR (Tele rehabilitation) OR (Tele-
rehabilitations)OR (Remote Rehabilitation) OR (Rehabilitation,
Remote) OR (Rehabilitations, Remote) OR (Remote
Rehabilitations) OR (Virtual Rehabilitation) OR
(Rehabilitation, Virtual)OR (Rehabil itations, Virtual) OR
(Virtual Rehabilitations) OR)) AND video conferencing) AND
((((telerehabilitation) OR (tele-rehabilitation) OR (tele rehabilita-
tion) OR (tele-rehabilitations) OR (remote rehabilitation) OR (re-
habilitation, remote) OR (rehabilitations, remote) OR (remote
rehabilitations) OR (virtual rehabilitation) OR (rehabilitation, vir-
tual) OR (rehabilitations, virtual) OR (virtual rehabilitations)))
AND pelvic floor muscle dysfunction); ((((Telerehabilitations)
OR (Tele-rehabilitation) OR (Tele rehabilitation) OR (Tele-
rehabilitations)OR (Remote Rehabilitation) OR (Rehabilitation,
Remote) OR (Rehabilitations, Remote) OR (Remote
Rehabilitations) OR (Virtual Rehabilitation) OR
(Rehabilitation, Virtual)OR (Rehabil itations, Virtual) OR
(Virtual Rehabilitations) OR)) AND video conferencing) AND
((((telerehabilitation) OR (tele-rehabilitation) OR (tele rehabilita-
tion) OR (tele-rehabilitations) OR (remote rehabilitation) OR (re-
habilitation, remote) OR (rehabilitations, remote) OR (remote
rehabilitations) OR (virtual rehabilitation) OR (rehabilitation, vir-
tual) OR (rehabilitations, virtual) OR (virtual rehabilitations)))
AND pelvic floor muscle dysfunction); (((telerehabilitation)
OR (t ele-rehabilitation) OR (tele rehabilitation) OR (tele-
rehabilitations) OR (remote rehabilitation) OR (rehabilitation, re-
mote) OR (re habilitations, remote) OR (remote rehabilitations)
OR (virtual rehabilitation) OR ( rehabilitation, virtual) OR (reha-
bilitations, virtual) OR (virtual rehabilitations))) AND pelvic
floor muscle dysfunction; (((telerehabilitation) OR (tele-
rehabilitation) OR (tele rehabilitation) OR (tele-rehabilitations)
OR (remote rehabilitation) OR (rehabilitation, remote) OR (reha-
bilitations, remote) OR (remote rehabilitations) OR (virtual reha-
bilitation) OR (rehabilitation, virtual) OR (rehabilitations, virtual)
OR (virtual rehabilitations))) AND sexual dysfunction;
(((telerehabilitation) OR (tele-rehabilitation) OR (tele rehabilita-
tion) OR (tele-rehabilitations) OR (remote rehabilitation) OR (re-
habilitation, remote) OR (rehabilitations, remote) OR (remote
rehabilitations) OR (virtual rehabilitation) OR (rehabilitation, vir-
tual) OR (rehabilitations, virtual) OR (virtual rehabilitations)))
AND pelvic pain; (((telerehabilitation) OR (tele-rehabilitation)
OR (tele rehabilitation) OR (tele-rehabilitations) OR (remote re-
habilitation) OR (rehabilitation, remote) OR (rehabilitations, re-
mote) OR (remote rehabilitations) OR (virtual rehabilitation) OR
(rehabilitati on, virtual) OR (rehabilitations, virtual) OR (virtual
rehabilitations))) AND urinary incontinence; (((telerehabilitation)
OR (t ele-rehabilitation) OR (tele rehabilitation) OR (tele-
rehabilitations) OR (remote rehabilitation) OR (rehabilitation, re-
mote) OR (re habilitations, remote) OR (remote rehabilitations)
OR (virtual rehabilitation) OR ( rehabilitation, virtual) OR (reha-
bilitations, virtual) OR (virtual rehabilitations))) AND Women’s
health; telerehabilitation) OR (tele-rehabilitation) OR (tele reha-
bilitation) OR (tele-rehabilitations) OR (remote rehabilitation)
OR (rehabilitation, remote) OR (rehabilitations, remote) OR (re-
mote rehabilitations) OR (virtual rehabilitation) OR (rehabilita-
tion, virtual) OR (rehabilitations, virtual) OR (virtual rehabilita-
tions) Telerehabilitation[MeSH Terms]Pelvic Prolapse;
(((((((Telehealth) AND Women’ s health)) AND
((telerehabilitation) OR (tele-rehabilitation) OR (tele rehabilita-
tion) OR (tele-rehabilitations) OR (remote rehabilitation) OR (re-
habilitation, remote) OR (rehabilitations, remote) OR (remote
rehabilitations) OR (virtual rehabilitation) OR (rehabilitation, vir-
tual) OR (rehabilitations, virtual) OR (virtual rehabilitations))))
AND ((v ideo confe rencing) AND pelvic floor muscle dysfunc-
tion))) AND (Pelvic Prolapse[MeSH Terms]); (((Pelvic
Prolapse) AND (Tele)) AND (Telerehabilitation[MeSH
Terms])) AND (Internet[MeSH Terms]); (telehealth) AND
women’s health; (((((telerehabilitation) OR (tele-rehabilitation)
OR (tele rehabilitation) OR (tele-rehabilitations) OR (remote re-
habilitation) OR (rehabilitation, remote) OR (rehabilitations, re-
mote) OR (remote rehabilitations) OR (virtual rehabilitation) OR
(rehabilitati on, virtual) OR (rehabilitations, virtual) OR (virtual
rehabilitations))) AND Women’s health)) AND telehealth; (vid-
eo conferencing) AND pelvic floor muscle dysfunction AND
Pelvic Prolapse; (((Telerehabilitations) OR (Tele-rehabilitatio n)
OR (Tele rehabilitation) OR (Tele-rehabilitations)OR (Remote
Rehabilitation) OR (Rehabilitation, Remote) OR
(Rehabilitations, Remote) OR (Remote Rehabilitations) OR
(Virtual Rehabilit ation) OR (Rehabilitation, Vi rtual)OR
(Rehabilitations, Virtual) OR (Virtual Rehabilitations) OR))
AND Pelvic Floor AND Pelvic Prolapse; Telerehabilitation
AND Internet AND Fecal Incontinence; Fecal incontinences
AND Tele; (((Telerehabilitations) OR (Tele-rehabilitation) OR
(Tele rehabilitation) OR (Tele-rehabilitations)OR (Remote
Rehabilitation) OR (Rehabilitation, Remote) OR
(Rehabilitations, Remote) OR (Remote Rehabilitations) OR
(Virtual Rehabilit ation) OR (Rehabilitation, Vi rtual)OR
(Rehabilitations, Virtual) OR (Virtual Rehabilitations) OR))
AND Pelvic Floor AND tele AND fecal incontinence;
Women’s Health AND Videoconferencing AND fecal
Incontinence; Fecal Incontinence AND in ternet.
EMBASE.
(Physioterapy OR Telerehabilitation) AND Women’S
AND Health AND ‘Sexual Dysf unction ’; (Physio AND
Terapy OR Telerehabilitation)AND Women’S AND Health
AND ‘Sexual Dysfunction’; (Physio AND Terapy OR
Telerehabilitation) AND Women’S AND Health AND
Urinary AND Incontinence; (Telerehabilitation OR Tele)
AND Women’ S AND Health AND Urinary AND
Incontinence;Physical AND Therapy AND
Telerehabilitation AND Women’S AND Health AND
Urinary AND Incontinence; Telerehabilitation AND Internet
Int Urogynecol J

AND Urinary AND Incontinence AND ‘Women’SHealth’;
Telerehabilitation AND Tele AND ‘Urine Incontinence’
AND ‘Women’S Health’; Telerehabilitation AND Tele
AND ‘ Pelvic Floor’ AND ‘ Women’ SHealth’ ;
Telerehabilitation AND Tele AND Pelvic AND Organ AND
Prolapse AND ‘Women’S Health’; Telerehabilitation AND
Tele AND Incontinence AND Urinary; (‘Telerehabilitation’/
Exp OR Telerehabilitation) AND Tele AND Continence;
(‘Videoconferencing’/Exp OR Videoconferencing) AND
Tele AND Pelvic AND Floor; Tele AND Sexual AND
Dysfunction AND Videoconferencing; (‘Telerehabilitation’/
Exp OR Telerehabilitation) AND Sexual AND Dysfunction
AND Videoconferencing; (‘Telehealth’/Exp OR Telehealth
OR Telerehabilitation:Ti) AND ‘Womens Health’ AND
‘ Pelvic Floor’ ;(‘ Videoconferencing’ /Exp OR
Videoconferencing) AND ‘Womens Health’ AND ‘Pelvic
Floor’;(‘Videoconferencing’/Exp OR Videoconferencing)
AND ‘ Womens Health’ AND ‘ Pelvic Floor’ ;
Telere habilitation AND ‘Muscle Dysfunction’ AND Tele;
Telerehabilitation AND Fecal AND Incontinence AND Tele
AND ‘Women’SHealth’; Telerehabilitation AND Tele AND
‘Women’SHealth’ AND Pelvic AND Pain; Telerehabilitation
AND Telehealth AND ‘Women’S Health’ AND Pelvic AND
Pain; (‘Vide oconferencing’/Exp OR Videoconferencing)
AND Telerehabilitation AND ‘Womens Health’ AND
‘Pelvic Floor’ ;(‘Internet’ /Exp OR Internet) AND
Telerehabilitation AND ‘Womens Health’ AND ‘Pelvic
Floor’;(‘Telerehabilitation’/Exp OR Telerehabilitation)
AND Telerehabilitation AND ‘Womens Health’ AND
‘ Pelvic Floor’ ;(‘ Telerehabilitation’ /Exp OR
Telerehabilitation) AND Telerehabilitation AND ‘Womens
Health’ AND ‘Pelvic Floor’;(‘Telerehabilitation’/Exp OR
Telerehabilitation) AND ‘ Womens Health’ ;
(‘Telerehabilitation’/E xp OR Telerehabi litation) AND
‘Pelvic Floor’;(‘Pelv ic Floo r’/Exp OR ‘Pelvic Floor’ OR
((‘ Pelvic’ /Exp OR Pelvic) AND Floor)) AND
Telerehabilitation
References
1. Digital Practice White Paper and Survey. http://www.inptra.org/
Resources/DigitalPracticeWhitePaperandSurvey.aspx. Accessed
30 April, 2020.
2. Dantas LO, Barreto RPG, Ferreira CHJ. Digital physical therapy in
the COVID-19 pandemic [published online ahead of print, 2020
May 1]. Braz J Phys Ther. 2020;S1413–3555(20):30402–0.
https://doi.org/10.1016/j.bjpt.2020.04.006.
3. Chartered Society of Physiotherapy. Remote service delivery op-
tions. https://www.csp.org.uk/news/coronavirus/remote-service-
delivery-options. Accessed 30 April, 2020.
4. Canadian Physiotherapy Association. Tele-Rehabilitation. https://
physiotherapy.ca/telerehabilitation. Accessed 30 April, 2020.
5. Conselho Federal de Fisioterapia e Terapia Ocupacional
(COFFITO). Resolução No 516, de 20 de março de 2020 -
Teleconsulta, Telemonitoramento e teleconsultoria; 2020. https://
www.coffito.gov.br/nsite/?p=15825.Accessed30April,2020.
6. Bø K, Mørkved S. Ability to contract the pelvic floor muscles. In:
Bø K, Berg hmans B, Mørkved S , Van Kampen M, editors.
Evidence-based physical therapy for the pelvic floor. Edinburgh:
Elsevier; 2015. p. 110–7.
7. Kegel AH. Stress incontinence and genital relaxation; a nonsurgical
method of increasing the tone of sphincters and their supporting
structures. Ciba Clin Symp. 1952;4(2):35–51.
8. Bump R, Hurt WG, Fantl JA, Wyman JF. Assessment of Kegel
exercise performance after brief verbal instruction. Am J Obstet
Gynecol. 1991;165:322–9. https://doi.org/10.1016/0002-9378(91)
90085-6.
9. Castro RA, Arruda RM, Zanetti MR, Santos PD, Sartori MG, Girão
MJ. Single-blind, randomized, controlled trial of pelvic floor mus-
cle training, electrical stimulation, vaginal cones, and no active
treatment in the management of stress urinary incontinence.
Clinics (Sao Paulo). 2008;63(4):465–72. https://doi.org/10.1590/
s1807-59322008000400009.
10. Bø K, Hagen RH, Kvarstein B, Jørgensen J, Larsen S. Pelvic floor
muscle exercise for the treatment of female urinary stress inconti-
nence: III. Effects of two different degrees of pelvic floor muscle
exercises. Neurourol Urodyn. 1990;9:489–502. https://doi.org/10.
1002/nau.1930090505.
11. Fitz FF, Gimenez MM, de Azevedo Ferreira L, Matias MMP,
Bortolini MAT, Castro RA. Pelvic floor muscle training for female
stress urinary incontinence: a randomised control trial comparing
home and outpatient training. Int Urogynecol J. 2020;31(5):989–
98. https://doi.org/10.1007/s00192-019-04081-x.
12. Felicíssimo MF, Carneiro MM, Saleme CS, Pinto RZ, da Fonseca
AM, da Silva-Filho AL. Intensive supervised versus unsupervised
pelvic floor muscle training for the treatment of stress urinary in-
continence: a randomized comparative trial. Int Urogynecol J.
2010;21(7):835–40. https://doi.org/10.1007/s00192-010-1125-1.
13. Bagg MK, McAuley JH. Correspondence: living systematic re-
views. J Phys. 2018;64(2):133. https://doi.org/10.1016/j.jphys.
2018.02.015.
14. Sherrington C, Herbert RD, Maher CG, Moseley AM. PEDro. A
database of randomized trials and systematic reviews in physiother-
apy. Man Ther. 2000;5(4):223–6. https://doi.org/10.1054/math.
2000.0372.
15. Osborne LA, Whittall CM, Emanuel R, Emery S, MD DPPR.
Randomized controlled trial of the effect of a brief telephone sup-
port intervention on initial attendance at physiotherapy group ses-
sions for pelvic floor problems. Arch Phys Med Rehabil. 2017;98:
2247–52. https://doi.org/10.1016/j.apmr.2017.03.033.
16. Carrión Pérez F, Rodríguez Moreno MS, Carnerero Córdoba L,
Romero Garrido MC, Quintana Tirado L, Garcí a Montes I.
Tratamiento de la incontinencia urinaria de esfuerzo mediante
telerrehabilitación. Estudio piloto [Telerehabilitation to treat stress
urinary incontinence Pilot study]. Med Clin (Barc). 2015;144(10):
445–
8. https://doi.org/10.1016/j.medcli.2014.05.036.
17. Kristjánsdóttir OB, Fors EA, Eide E, et al. A smartphone-based
intervention with diaries and therapis t-feedback to reduce
catastrophizing and increase functioning in women with chronic
widespread pain: randomized controlled trial. J Med Internet Res.
2013;15(1):e5. https://doi.org/10.2196/jmir.2249.
18. Kristjánsdóttir ÓB, Fors EA, Eide E, et al. A smartphone-based
intervention with diaries and therapist feedback to reduce
catastrophizing and increase functioning in women with chronic
widespread pain. Part 2: 11-month follow-up results of a random-
ized trial. J Med Internet Res. 2013;15(3):e72. https://doi.org/10.
2196/jmir.2442.
Int Urogynecol J
