RES E AR C H A R T I C L E Open Access
Can virtual reality improve traditional
anatomy education programmes? A mixed-
methods study on the use of a 3D skull
model
Shi Chen
1,2†
, Jiawei Zhu
3†
, Cheng Cheng
3†
, Zhouxian Pan
3
, Lingshan Liu
3
, Jianhua Du
3
, Xinhua Shen
4
, Zhen Shen
5
,
Huijuan Zhu
1
, Jihai Liu
2,6
, Hua Yang
2,7
, Chao Ma
4
and Hui Pan
1,8*
Abstract
Background: Realistic, portable, and scalable lectures, cadaveric models, 2D atlases and computer simulations are
being combined more frequently for teaching anatomy, which result in major increases in user satisfaction.
However, although digital simulations may be more portable, interesting, or motivating than traditional teaching
tools, whether they are superior in terms of student learning remain unclear. This paper presents a study in which
the educational effectiveness of a virtual reality (VR) skull model is compared with that of cadaveric skulls and
atlases. The aim of this study was to compare the results of teaching with VR to results of teaching with traditional
teaching methods by administering objective questionnaires and perception surveys.
Methods: A mixed-methods study with 73 medical students was conducted with three different groups, namely,
the VR group (N = 25), cadaver group (N = 25) and atlas group (N = 23). Anatomical structures were taught through
an introductory lecture and model-based learning. All students completed the pre- and post-intervention tests,
which comprised a theory test and an identification test. The theory test consisted of 18 multiple-cho ice questions,
and the identification test consisted of 25 fill-in-the-blank questions.
Results: The participants i n all three groups had significantly higher total scores on the post-intervention test than on the
pre-intervention test; the post-intervention test score in the VR group was not statistically significantly higher than the
post-intervention test score of the other groups (VR: 30 [IQR: 22–33.5], cadaver: 26 [IQR: 20–31.5], atlas: 28[IQR: 20–33]; p >
0.05). The participants in the VR and cadaver groups provided more positive feedback on their learning models than the
atlas group (VR: 26 [IQR: 19–30], cadaver: 25 [IQR: 19.5–29.5], atlas: 12 [IQR: 9–20]; p <0.001).
(Continued on next page)
© The Author(s). 2020 Open Access This article is licensed under a Creative Commons Attribution 4.0 International License,
which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if
changes were made. The images or other third party material in this article are included in the article's Creative Commons
licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons
licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain
permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the
data made available in this article, unless otherwise stated in a credit line to the data.
†
Shi Chen, Jiawei Zhu and Cheng Cheng contributed equally to this work.
1
Department of Endocrinology, Endocrine Key Laboratory of Ministry of
Health, Peking Union Medical College Hospital (PUMCH), Chinese Academe
of Medical Sciences & Peking Union Medical College (CAMS & PUMC), Beijing
100730, China
8
Medical Department, PUMCH, CAMS & PUMC, Beijing 100730, China
Full list of author information is available at the end of the article
Chen et al. BMC Medical Education (2020) 20:395
https://doi.org/10.1186/s12909-020-02255-6
(Continued from previous page)
Conclusions: The skull virtual learning resource (VLR) was equally efficient as the cadaver skull and atlas in teaching
anatomy structures. Such a model can aid individuals in understanding complex anatomical structures with a higher level
of motivation and tolerable adverse effects.
Keywords: Virtual reality, Anatomy, Medical education
Background
Although anatomy serves as the basis for other medical
courses for medical students [1], universities have de-
creased the hours allocated to anatomy education in
favour of applied clinical work [2]. Medical students
need to supplement their anatomy education with plenty
of traditional resources, including cadaveric dissection,
preserved specimens, and vario us 2-dimensional (2D)
image representations (e.g. textbook illustrations, atlases,
and tomographic scans) [3]. Recent advancements in
computer technology have led to many different forms
of digital anatomy simulations [4]. Among them, virtual
reality (VR) technology is one of the most promising
teaching tools in medical education. VR can be used to
deliver a highly immersive experience through head-
mounted displays (HMDs) and a less immersive experi-
ence through a desktop system [5]. A wide range of vir-
tual learning resources (VLRs) have been developed that
use 3-dimensional (3D) visualization technologies to
supplement and even replace traditional instructional
materials such as cadaver dissections [3]. Users can
interact with vivid imagery for an active and self-
directed learning experience without the limitations of
ethical concerns and donation shortages [ 6, 7] or having
to enter an anatomy laboratory [4]. In a few studies, the
educational value of VLRs has been compared with that
of conventional methods, and the results are generally
inconsistent. When used either alone or to complement
traditional written and online materials, VLRs showed
better or similar effectiveness in terms of enabling stu-
dents to learn anatomy [2, 8–11]. More importantly,
VLRs are rated as more interesting and engaging [8], en-
joyable [8, 9, 11], motivating [8, 12–14] and useful for
understanding spa tial relationships [11, 13, 15] than
traditional tools. There is an inherent appeal in these
newer and more advanced visualizations in addition to
their novelty [4]. However, studies have shown that
compared with cadaver dissection and physical modes,
VLRs are less effective in improving learning outcomes
[16, 17]. The lack of tactile experience is regarded as a
disadvantage.
Although current studies suggest that VLRs cannot re-
place cadaver and physical models, they are perceived as
promising supplementary resources in anatomy educa-
tion. It is therefore important to evaluate the evidence
from different aspects. However, current researches are
largely focused on the comparison between VLRs and
2D textbooks, online materials or physical models.
Petersson et al. [16] and Codd et al. [17] both compared
VLRs with cadaver dissection, but neither study used
VLRs to deliver a highly immersive experience. Recent
studies by Birbara et al. [18] and Shao et al. [10] provide
a fully immersive experience, but neither of the research
groups compared VLRs with cadave r dissection, and the
VLR group used only perception questionnaires. Object-
ive assessments are crucial to evaluating participant s’
performance, in which the identification test is consid-
ered to be a predictor of imp roved learning outcomes
following 3D learning [19, 20]. Therefore, immersive
VLRs and traditiona l teaching modalities, such as ca-
daver dissection and 2D atlases, should be further com-
pared, and the different aspects of the assessments
should also be considered to evalu ate the impact of
VLRs on anatomy education.
Aim and hypothesis
Neurosurgery comprises some of the most challenging
surgical procedures, and mastering the intricacies of cra-
nial anatomy is a career-long endeavour for every neuro-
surgeon [10]. In this study, a coloured and detachable
skull VLR was constructed. The aim of this study was to
compare the results of the skull VLR with the cadaver
skull and a 2D atlas for anatomy education by adminis-
tering objective questionnaires and perception surveys.
Our hypothesis was that the skull VLR and cadaveric
skull groups might have similar performance in the ob-
jective tests, and that students would show a more posi-
tive attitude towards their learning material than the
atlas group.
Materials and method s
3D skull model based on VR technology
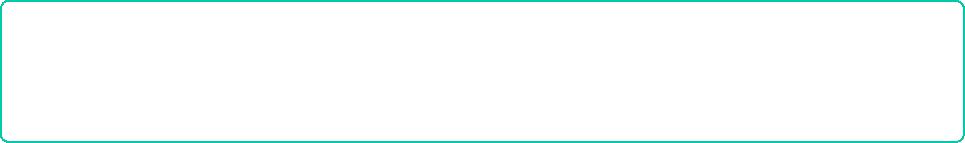
The virtual 3D skull model used in this study was con-
structed from computed tomography (CT) scans of a
human skull from the Peking Union Medical College
(PUMC) Anatomy Teaching Collection (Fig. 1). The CT
scans were impo rted into Mimics 17.0 (Materialise NV,
Leuven, Belgium) and con verted into stereolithography
(STL) files. The method used to create a 3D model from
CT scans was previously published by Shui et al. [21].
Several defective structures (ethmoid plate, crista galli,
anterior clinoid process and inferior orbital fissure) on
Chen et al. BMC Medical Education (2020) 20:395 Page 2 of 10
the 3D skull model were modified by using 3D Studio
Max 2016 (Autodesk Inc., San Rafael, CA). In addition,
each bone was isolated from the entire skull and painted
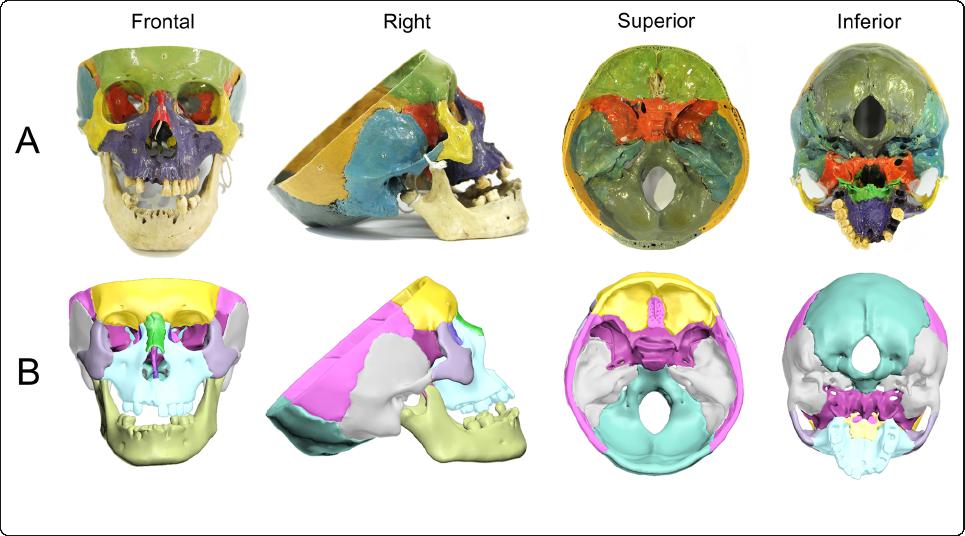
in a different colour (Fig. 2 c & d). The model was then
imported into the Unreal Engine VR platform (Fig. 2a)
through the HTC VIVE software development kit (High
Technology Computer Corporation, Taiwan) and Unreal
Engine 4.15 (Epic Games Inc., Cary, NC), which is com-
patible with HTC VIVE CE (High Technology Computer
Corporation, Taiwan), a VR HMD with a resolution of
2160 × 1200. Users could rotate and scale the model
through handheld controllers. In addition, each cranial
bone could be isolated from all other bones, which al-
lows the user to view an individual selected bone and its
position in space relative to the other bones. When the
isolated structure was placed back in its original pos-
ition, the model was reset.
Participants
Seventy-four clinical undergraduates from PUMC who
had just finished a 2.5-year pre-medical programme at
Tsinghua University were recruited. Thes e students
would begin their undergraduate stage of medicine in
the subsequent 5.5 years, from the basic study of anat-
omy to clinical internships. The anatomy course com-
bines regional and systematic anatomy and requires 144
study hours for each student. Every theoretical lecture is
followed by a cadaver dissection teaching of equ ivalent
time. There are a theoretical test and an identification
test for objective assessment at the end of the course.
The students were randomly divided into three groups,
namely, the skull VLR group (VR group, n = 25), cadav-
eric skull group (cadaver group, n = 25), and 2D atlas
group (atlas group, n = 24). Seventy-three participants
completed the trial, while one participant in the atlas
group dropped out of the study for personal reasons be-
fore the pre-intervention test.
Ethical approval
This study was approved by the Institutional Review
Board of the Institute of Peking Union Medical College
Hospital (PUMCH) (Project No: ZS-1724).
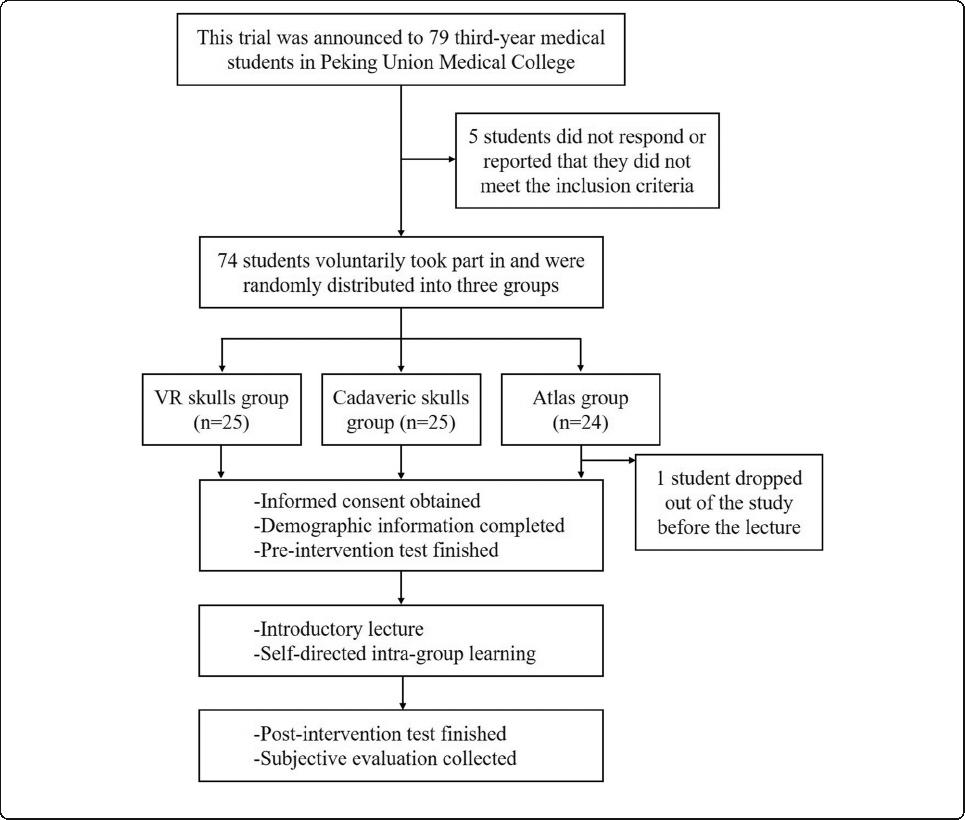
Design
A flowchart of the study design is displayed in Fig. 3. All
participants finished the pre-intervention tests. Then,
they attended a 30-min PowerPoint-based introductory
lecture on cranial anatomy, which included the charac-
teristics of each cranial bone, feature structures and
spatial relationships. The lecture was taught by a teacher
from PUMC whom the students had not met before.
During the lecture, each participant received a single
sheet of pape r with the teaching outline, which could
also be used for note-taking. Afterwards, the three
groups were assigned to three separate rooms for a 30-
min self-directed learning session that used skull VLR,
cadaveric skulls, and 2D atlases. The students in the VR
group received a 2-min instruction about the manipula-
tion of the VR equipment before learning. Study men-
tors were assigned to each room to prevent intragroup
Fig. 1 Photos of the cadaveric skull and skull VLR. a From left to right, the cadaveric skull is shown in the frontal, right, superior and inferior
views. b From left to right, the skull VLR is shown in the frontal, right, superior and inferior views
Chen et al. BMC Medical Education (2020) 20:395 Page 3 of 10
communication and were forbidden to answer questions
related to anatomy. The participants took turns so that
each participant had 7.5 min to manipulate and observe
the model in the first perspective, and they observed the
3D model on the computer screen for the remaining
22.5 min. The participants in the cadaver and atlas
groups also had the same amount of time to hold the ca-
daver skull or atlas, while the other participants could
only observe, without manipulation. To compensate for
the inability to view the teaching outline on paper in the
simulated environment, a projector was used to project
the teaching outline on a screen (Fig. 2b). A post-
intervention test was conducted immediately after the
learning session to evaluate the educational efficacy of
each model. Finally, each participant completed a per-
ception survey.
The pre- and post-intervention tests comprised the
same set of theory tests and identification tests (Supple-
mentary file 1.1 & 1.2). The theory test consisted of 18
multiple-choice questions tha t mainly covered basic
knowledge on the skull. Each correct answer was
awarded 1 point, and the examination lasted 15 min.
The id entification test consisted of 25 fill-in-the-blank
questions on labelled anatomical structures of the skull.
All structures were labelled on the cadaveric skulls. The
participants had 45 s to observe each structure and write
down its name. Each correct answer was awarded 1
point. The content was based on the syllabus from the
PUMC anatomy course, and all the test questions are
available in Supplementary file 1.
To assess the potentia l efficacy of the teaching tools,
in addition to the objective learning efficiency deter-
mined by the test scores, a perception survey was de-
signed (Supplementary file 1.3). The questions were
based on those included in several previous studies con-
ducted to evaluate the efficacy of other 3D models [8,
19, 22]. The perception survey used in this study con-
sisted of five parts that addr essed the participants’ enjoy-
ment, learning efficiency, attitude, intention to use, and
the tool’s authenticity, and a standard five-point Likert
scale was used to quantify the responses (1-strongly dis-
agree, 5-strongly agree with the statement).
Data collection and marking
Demographic information, including each participant’s
age, sex, self-reported VR headset experience and video
game experience, was collected during the trial. The par-
ticipants recorded their group and individual identifica-
tion numbers on the sign-in sheet. The previous grade
point average (GPA) of each participant was obtained
from the grade counsellor. The demographic and group-
ing information were hidden from the test mentor, study
Fig. 2 Photos of the simulation classroom and the skull VLR. a The entire classroom, in which a skull is placed on a table in the front of the
classroom, the other skull is placed on a table in the middle of the classroom, and pictures of the human skeleton are placed in front of the
window. b The skull VLR and projection screen. c The frontal bone separated from the entire skull. d All the bones separated, with the bright
white ball representing the center of the original skull
Chen et al. BMC Medical Education (2020) 20:395 Page 4 of 10
mentor and study staff until the trial was completed. The
study staff scored each answer sheet, and the results were
reviewed by the investigators (Zhu J and Cheng C) twice.
By using the Chen et al.’s[19] mean total scores and the
variance data of the post-intervention test, power calculations
were performed for this study. The calculations revealed that
26 students were required per group (78 students total) to
achieve 80% power to detect a 10% change in the post-
intervention total scores at an alpha level of 0.05.
Statistical analysis
The previous GPA, test scores and perception survey
scores were expressed as medians (interquartile ranges
(IQRs)), and the categorical variables were expressed as
numbers (%). The participants’ ages were expressed as
means (±SDs). A p-value of < 0.05 was considered to in-
dicate statistical significance. Statistical analysis was per-
formed with SPSS 23.0 (IBM Corp, Armonk, NY).
The data distributions were assessed with the
Kolmogorov-Smirnov test. The between-group differences
in the pre- and post-intervention test scores, changes in the
scores, and perception survey scores were assessed with the
Kruskal-Wallis H test because they were found to be non-
normally distributed. If there was a significant difference
with the Kruskal-Wallis H test, the Mann-Whitney U test
was employed for pairwise comparisons. The participants’
ages were compared with ANOVA. The categorical vari-
ables, except for video game experience, were compared
with the chi-square test; video game experience was com-
pared with Fisher’s exact test.
Results
Participant demographics
A total of 73 third-year medical students (39 females,
53.42%) were included in the study (Table 1). Most par-
ticipants were 20 or 21 years old. There were no
Fig. 3 Flowchart of the study design
Chen et al. BMC Medical Education (2020) 20:395 Page 5 of 10
statistically significant differences across the 3 groups in
terms of gender, age, previous GPA in the pre-med
programme at Tsinghua University, VR experience or
video game experience (all p > 0.05).
Comparison of the test score s across groups
The scores for the theory test and identification test
were included in the total scores. The maximum scores
of the theory test, identif ication test, and both tests to-
gether were 18, 25, and 43 points, respectively. A within-
subject analysis showed overall improvement in the test
scores from before to after the intervention, and the
magnitude of improvement was significantly different
across the three groups (p < 0.001). Table 2 displays the
results of the pre- and post-intervention tests.
No statistically significant difference was revealed across
the three groups in the pre-intervention tests (p >0.05for
the total score, theory score, and identification score). In
terms of the post-intervention test, there were no statisti-
cally significant differences across the three groups in ei-
ther the total score or theory score (all p >0.05). The
participants in the VR group performed better in the iden-
tification test than the cadaver and atlas groups (Fig. 4), al-
though with no significance (VR: 15 [IQR: 10–18],
cadaver: 12 [IQR: 8–15.5], atlas: 13 [IQR: 8–18]; p >0.05).
The differences between the pre- and post-
intervention test scores of the individual students were
considered by using the change in scores. Kruskal-Wallis
H analysis revealed that the changes in the scores were
not significantly different across the three groups (p >
0.05 for the changes in the total, theory, and identifica-
tion scores), as shown in Fig. 4.
Results of the perception survey
Comparisons of the results of the perception survey are
shown in Table 3. Overall, the participants in the VR
and cadaver groups found their assigned learning models
to be more enjoyable (VR: 4 [IQR: 3–5], cadaver: 4 [IQR:
3–5], atlas: 2 [IQR: 1–3]; p < 0.001), more interesting
(VR: 4 [IQR: 3–5], cadaver: 4 [IQR: 3–4.5], atlas: 2 [IQR:
1–3]; p < 0.001), more authentic (VR: 4 [IQR: 3–5], ca-
daver: 4 [IQR: 3–5], atlas: 2 [IQR: 1–3]; p < 0.001), and
more efficient for memorization (VR: 3 [IQR: 2–4], ca-
daver: 3 [IQR: 3–4], atlas: 2 [IQR: 1–4]; p < 0.001) and
spatial understanding (VR: 4 [IQR: 4–5], cadaver: 4
[IQR: 3–4.5], atlas: 1 [IQR: 1–3]; p < 0.001). The VR and
cadaver groups reported a higher intention to include
the study material for use in standard anatomy educa-
tion (VR: 3 [IQR: 2–4], cadaver: 4 [IQR: 2.5–4], atlas: 1
[IQR: 1–2]; p < 0.001).
Discomfort during the learning session
During the learning process, discomfort including head-
ache, blurred vision and nausea were evaluated in the
three groups (Supplementary file 2). Although the partici-
pants in the VR group exhibited these adverse effects
more frequently than in the other 2 groups, no significant
difference was found (VR group: 24%, cadaver group: 12%,
atlas group: 8.7%, p > 0.05). Additionally, in the VR group,
the total scores of the post-intervention tests did not vary
in the participants with and without discomfort (30 [IQR:
19.25–32.5] vs. 30 [IQR: 22–34], p >0.05).
Discussion
This is the first study to compare VLR with two different
traditional teaching methods in a randomized controlled
study design, including both objective assessments and
perception surveys, namely, “various question types” in
previous research [19]. The results of the object ive as-
sessment demonstrated that the skull VLR had the same
efficiency as the cadaver skull and atlas in enabling stu-
dents to learn anatomy, despite the relative simplicity of
the model used in this study. The post-intervention identifi-
cation scores were higher in the VR group, although not sig-
nificantly, compared with the other two groups. This result
was consistent with the advantages of VR in stereoscopic
Table 1 Demographic information in the three groups.
a
Chi-square test.
b
ANOVA.
c
Kruskal-Walis H.
d
Fisher’s Exact test
VR skulls
(N = 25)
Cadaveric skulls
(N = 25)
Atlas
(N = 23)
p-value
Gender [n (%)]
Male 9 (36%) 13 (52%) 12 (52.17%) 0.425
a
Female 16 (64%) 12 (48%) 11 (47.83%)
Age (Median [IQR]) 21.22 ± 0.69 21.15 ± 0.54 21.19 ± 0.78 0.948
b
Previous GPA (Median [IQR]) 3.28 [3.14–3.43] 3.30 [3.06–3.47] 3.23 [3.21–3.40] 0.780
c
VR headset experience [n (%)] 9 (36%) 7 (28%) 7 (30.43%) 0.823
a
Video game experience [n (%)]
Always 2 (8%) 0 (0%) 1 (4.35%) 0.696
d
Occasionally 4 (16%) 4 (16%) 2 (8.70%)
Rarely 19 (76%) 21 (84%) 20 (86.95%)
Chen et al. BMC Medical Education (2020) 20:395 Page 6 of 10

Table 2 Pre- and post-intervention tests score in the three groups. Full scores of theory test, identification test, and total score were
18, 25, and 43 points, respectively. The median and quartiles of the total scores were not simply equal to the sum of the theory
score and the identification score.
c
Kruskal-Walis H
VR skulls
(N = 25)
Cadaveric skulls
(N = 25)
Atlas
(N = 23)
p-value
Pre-intervention score (Median [IQR])
Total 9 [6.5–13] 8 [7–11] 10 [7–14] 0.634
c
Theory test 7 [5–9] 7 [5–9] 7 [6–10] 0.667
c
Identification test 3 [1.5–4.5] 2 [0.5–3] 2 [1–5] 0.176
c
Post-intervention score (Median [IQR])
Total 30 [22–33.5] 26 [20–31.5] 28 [20–33] 0.571
c
Theory test 15 [12.5–16] 14 [12.5–15.5] 14 [11–16] 0.824
c
Identification test 15 [10–18] 12 [8–15.5] 13 [8–18] 0.511
c
Change in score (Median [IQR])
Total 18 [14.5–21.5] 18 [12.5–21.5] 16 [10–20] 0.317
c
Theory test 7 [5–9] 7 [4.5–10] 6 [3–8] 0.524
c
Identification test 12 [8–12] 9 [7.5–13.5[ 9 [7–13] 0.278
c
Fig. 4 Comparison across the three groups in the post-intervention test scores and changes in scores. There were no statistically significant
differences across the three groups in the post-intervention test scores and changes in scores
Chen et al. BMC Medical Education (2020) 20:395 Page 7 of 10
observation and operation, which incorporated the intrinsic
spatial relationships of the anatomical sites studied and may
thus confer a spatial knowledge advantage [11]. The results
of the perception survey in the VR and cadaver groups also
showed a more positive attitude towards the learning models
than the results of the 2D atlas group, which indicated that
the VR and cadaver groups had similar levels of enjoyment,
learning efficacy and authenticity. Novel interventions usually
spark participants’ curiosity and lead to better results [4], and
all participants in the VR group were highly enthusiastic to
promote the use of this skull VLR in anatomy education.
Similarly, previous studies that have compared a 3D VR
model with traditional 2D materials also reported that VR
wasconsideredtobeamoreenjoyableandusefuleduca-
tional tool [8, 11, 23].
Cadavers offer high levels of realism, haptic feedback, and
theopportunitytouserealinstruments and tools, which was
found to be superior to atlas models in several previous stud-
ies [24–26], particularly in surgery [ 27]. In our trial, the
scores of the cadaver skull group showed no statistically sig-
nificant differences from the scores of the atlas group. This
discrepancy might partially result from structural variations
and small damages of the cadaveric skulls and the negative
psychological reactions from participants triggered by the ca-
daveric skulls [28, 29]. In addition, we combined lecture and
model learning to simulate the real learning process. The lec-
tures allowed the participants to learn important information
for the tests and narrowed the differences across the three
groups. Moreover, exposure to the pre-intervention test will
affect performance on an identical post-intervention test
through familiarity with the questions and may also influence
learning during the intervention [30].
3D VLRs, which provide rapid and feedback-based modifi-
cations, offer an opportunity for repetitive practice [23]. An-
other advantage of VLRs is that students can observ e and
receive instant visual feedback based on predefined practical
tasks [31]. Critics have argued that this approach lacks expert
guidance during the learning process, which plays an import-
ant role in forming the basic framework [32]. In fact, teachers
can also assess students’ learning performance and mistakes
through digital reports to further improve students’ skills.
Moreover, the participants in our trial conducted self-
learning in the absence of guidance and gained substantial
progress in learning anatomical knowledge, which is consist-
ent with the results in a previous study [33]. It has been sug-
gested that self-learning in private places is a feasible way to
implement VR simulation learning without constraints of the
place or time provided for learning [33]. In addition, 3D
models are likely to enhance rather than replace lecture-
based teaching by experts [23]. Individuals can first practice
with a VR simulation rather than with cadavers so that they
can repeat the procedures and acquire basic skills before
using expensi ve laboratory facilities [33]. Our study incorpo-
rated a room-scale HMD unit, which was available for the in-
dividuals. With this unit, many more manipulations can be
easily achieved, such as rotating to a suitable view, segment-
ing a single bone and scaling up the model, which makes it a
better tool for understanding difficult anatomical structures.
This HMD unit provides a completely immersive experience
with a high-resolution display, a high refresh rate, and highly
precise, low-latency constellation head tracking.
However, adverse effects caused by the highly immer-
sive experience and the device being positioned in front
of the eyes were regarded as negative aspects of the
VLRs [18]. Adverse effects, including headaches, dizzi-
ness, sore eyes, blurred vision and motion sickness, have
been reported [2, 34, 35 ]. A previous study reported a
high adverse effect rate in a VR group (headaches 25%;
blurred vision 35%) [2], but this rate was lower in our
trial (headaches 20%, blurred vision 4%). It can be in-
ferred that the discomfort caused by the virtual environ-
ment could be relieved with increased resolution and
lower latency. Newer VR designs are being designed to
overcome motion sickness and other VR-associated ad-
verse effects. These designs include grounding the user
by allowing their eyes to fix on a constant object such as
a virtual nose or hand and decoupling the axes of move-
ment from the visual plane [18].
In addition to physical discomfort, the high degree of
immersion in a stereoscopic environment and the novel
Table 3 Results of perception survey in the three groups. Full score of perception survey is 35.
c
Kruskal-Walis H.
*
p < 0.05
VR skulls
(N = 25)
Cadaveric skulls
(N = 25)
Atlas
(N = 23)
p-value
Enjoyment Enjoyable 4 [3–5] 4 [3–5] 2 [1–3] < 0.001
c,*
Interest 4 [3–5] 3 [3–4.5] 2 [1–3] < 0.001
c,*
Authenticity 3 [2.5–4] 3 [3–4] 2 [1–3] 0.001
c,*
Learning Efficiency Memorize 3 [2–4] 3 [3–4] 2 [1–4] 0.029
c,*
Spatial 4 [4–5] 4 [3–4.5] 1 [1–3] < 0.001
c,*
Attitude 3 [2–3] 3 [2–4] 1 [1–2] < 0.001
c,*
Intention to use 3 [2–4] 4 [2.5–4] 1 [1–2] < 0.001
c,*
Total 26 [19–30] 25 [19.5–29.5] 12 [9–20] < 0.001
c,*
Chen et al. BMC Medical Education (2020) 20:395 Page 8 of 10

experience of an immersive learning might make the
learning process more mentally taxing [11, 15]. Khot et al.
suggested that the extraneous load of the virtual delivery
modalities might contribute to the worse performance of
students who used these modalities than students who
used physical models [36]. Birbara et al. also found that
students with minimal prior anatomy knowledge in a
stereoscopic cohort had a higher cognitive load [18]. With
no prior knowledge, the participants in our study might
have experienced a greater mental burden, which under-
mined their learning efficiency in the learning session.
Although commercially available and low-cost HMDs
have further enhanced the opportunities for a truly
interactive virtual experience [37], the cost of VLR as a
supplement should be noted. Each set of VR equipment
cost approximately 700 dollars in our study, and it requires
related software, computer hardware and technicians for
its maintenance [38]. Considering the benefits of improved
learning, repeated use, and versatility, VR can reduce the
costs of laboratory material, supervisor staff and even
simulated patients. In general, the cost-benefit trade-off for
these expensive technologies is likely to vary based on
institutional goals and resources [39].
Limitations
Our study had seve ral limitations. First, this is a single-
institution study with a small sample size that included
only 73 participants, which was close to but smaller than
the expected sample size. Further studies with larger
sample sizes are needed to examine a broader spectrum
of medical personnel including resident physicians, nurs-
ing students and related educators. Second, the self-
directed learning session was limited to 30 min in our
study. The participants in the VR group only received a
2-min instruction for the VR equipment manipulation
before the learning session. To reduce the mental bur-
den, prior acquaintance with a virtual environment may
be essential in future study designs. Third, as the pre-
and post-intervention tests were identical, probability
existed that the participants might have purposely fo-
cused on the questions in the pre-intervention tests dur-
ing the 30-min learning session, which may have
influenced their performance in the post-intervention
tests. Longer learning sessions should be considered in
future studies. Finally, this study directly compared VLR
with other resources and only combined VLR with trad-
itional lecture. Further studies are needed to identify the
optimal combination of VLRs with various teaching
methods such as cadaver dissection to fully reflect their
effectiveness as a supplementary aid in medical teaching.
Conclusion
In this study, the skull VLR was equally efficient with cadaver
skull and atlas in teaching anatomy structures. Such a model
can aid individuals in understanding complex anatomical
structures with a high level of motivation and tolerable ad-
verse effects. Advances in 3D digital technology have enabled
the development of more sophisticated and realistic VLRs,
which provide opportunities for its use in traditional anat-
omy teaching settings as a powerful supplement. Future gen-
erations of medical students may benefit from these
technologies at the earliest stages of their learning, from VR
anatomy models to patient-specific VR simulations, as
needed. Additional studies with larger sample sizes are re-
quired not only to evaluate the teaching effectiveness of
VLRs in a more comprehensive frame but also to investigate
the optimal combinations of VLRs with traditional medical
education.
Supplementary information
Supplementary information accompanies this paper at https://doi.org/10.
1186/s12909-020-02255-6.
Additional file 1.
Abbreviations
VR: Virtual Reality; VLR: Virtual Learning Resource; 2D: Two-dimensional;
3D: Three-dimensional; STL: Stereolithography; HMD: Head-mounted Display;
GPA: Grade Point Average
Acknowledgements
The authors appreciate the support from Mr. Zhang Di, Mrs. Li Wenting and
other members in Department of Anatomy in PUMC for provision of
cadaveric materials and test questions, and all participants from third grade
of eight-year program of clinical medicine in PUMC.
Authors’ contributions
S.C. and H.P. conceived and designed the trial. S.C., J.Z. and C.C. drafted the
manuscript. J.Z., C.C., Z.P., L.L., J.D. and X.S. conducted the experiment and
analyzed and interpreted the results. J.L. and Z.S. constructed the model. H.Y.
designed the questionnaires and led the data collection. H.P. and H.Y.
supervised the study. H.Z. and C.M. reviewed and revised the manuscript. All
authors reviewed and approved the final version.
Funding
This work was supported by grants from funds for Young Teachers Training
Program (No.2014zlgc0721), and Education Reform Program
(No.2014zlgc0141) of Peking Union Medical College. There was no financing
from public funds or from third parties.
Availability of data and materials
The datasets used and analysed during the current study are available from
the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the Institute of
Peking Union Medical College Hospital (PUMCH) (Project No: ZS-1724), and
written informed consent obtained from all the participants. Study methods
were performed in accordance with approved guidelines.
Consent for publication
Not applicable, no individual person’s data in any form.
Competing interests
The authors declare that they have no competing interests.
Author details
1
Department of Endocrinology, Endocrine Key Laboratory of Ministry of
Health, Peking Union Medical College Hospital (PUMCH), Chinese Academe
Chen et al. BMC Medical Education (2020) 20:395 Page 9 of 10
of Medical Sciences & Peking Union Medical College (CAMS & PUMC), Beijing
100730, China.
2
National Virtual Simulation Laboratory Education Center of
Medical Sciences, PUMCH, CAMS & PUMC, Beijing 100730, China.
3
Eight-year
Program of Clinical Medicine, PUMCH, CAMS & PUMC, Beijing 100730, China.
4
Department of Human Anatomy, Histology and Embryology, Institute of
Basic Medical Sciences, Neuroscience Center, Chinese Academy of Medical
Sciences, School of Basic Medicine, Peking Union Medical College, Beijing
100005, China.
5
The State Key Laboratory of Management and Control for
Complex Systems, Institute of Automation, Chinese Automation, Chinese
Academy of Sciences (CASIA), Beijing 100190, China.
6
Department of
Emergency, PUMCH, CAMS & PUMC, Beijing 100730, China.
7
Department of
Otolaryngology-Head and Neck Surgery, PUMCH, CAMS & PUMC, Beijing
100730, China.
8
Medical Department, PUMCH, CAMS & PUMC, Beijing
100730, China.
Received: 8 February 2020 Accepted: 24 September 2020
References
1. Turney BW. Anatomy in a modern medical curriculum. Ann R Coll Surg
Engl. 2007;89(2):104–7.
2. Moro C, Stromberga Z, Raikos A, Stirling A. The effectiveness of virtual and
augmented reality in health sciences and medical anatomy. Anat Sci Educ.
2017;10(6):549–59.
3. Preim B, Saalfeld P. A survey of virtual human anatomy education systems.
Comput Graph. 2018;71:132–53.
4. Wainman B, Pukas G, Wolak L, Mohanraj S, Lamb J, Norman GR. The critical
role of stereopsis in virtual and mixed reality learning environments. Anat
Sci Educ. 2020;13(3):401–12.
5. Suh A, Prophet J. The state of immersive technology research: a literature
analysis. Comput Hum Behav. 2018;86:77–90.
6. Gartner LP. Anatomical sciences in the allopathic medical school curriculum
in the United States between 1967-2001. Clin Anat. 2003;16(5):434–9.
7. Korf HW, Wicht H, Snipes RL, Timmermans JP, Paulsen F, Rune G, Baumgart-
Vogt E. The dissection course - necessary and indispensable for teaching
anatomy to medical students. Ann Anat. 2008;190(1):16–22.
8. Stepan K, Zeiger J, Hanchuk S, Del Signore A, Shrivastava R, Govindaraj S,
Iloreta A. Immersive virtual reality as a teaching tool for neuroanatomy. Int
Forum Allergy Rhinol. 2017;7(10):1006–13.
9. Preece D, Williams SB, Lam R, Weller R. "Let's get physical": advantages of a
physical model over 3D computer models and textbooks in learning
imaging anatomy. Anat Sci Educ. 2013;6(4):216–24.
10. Shao X, Yuan Q, Qian D, Ye Z, Chen G, le Zhuang K, Jiang X, Jin Y, Qiang D.
Virtual reality technology for teaching neurosurgery of skull base tumor.
BMC Med Educ. 2020;20(1):3.
11. Kockro RA, Amaxopoulou C, Killeen T, Wagner W, Reisch R, Schwandt E,
Gutenberg A, Giese A, Stofft E, Stadie AT. Stereoscopic neuroanatomy lectures
using a three-dimensional virtual reality environment. Ann Anat. 2015;201:91–8.
12. Battulga B, Konishi T, Tamura Y, Moriguchi H. The effectiveness of an
interactive 3-dimensional computer graphics model for medical education.
Interact J Med Res. 2012;1(2):e2.
13. Ferrer-Torregrosa J, Torralba J, Jimenez MA, García S, Barcia JM. ARBOOK:
development and assessment of a tool based on augmented reality for
anatomy. J Sci Educ Technol. 2014;24(1):119–24.
14. Ruisoto P, Juanes JA, Contador I, Mayoral P, Prats-Galino A. Experimental
evidence for improved neuroimaging interpretation using three-
dimensional graphic models. Anat Sci Educ. 2012;5(3):132 – 7.
15. Ferrer-Torregrosa J, Jimenez-Rodriguez MA, Torralba-Estelles J, Garzon-
Farinos F, Perez-Bermejo M, Fernandez-Ehrling N. Distance learning ects and
flipped classroom in the anatomy learning: comparative study of the use of
augmented reality, video and notes. BMC Med Educ. 2016;16(1):230.
16. PeterssonH,SinkvistD,WangC,SmedbyO.Web-basedinteractive3D
visualization as a tool for improved anatomy learning. Anat Sci Educ. 2009;2:61–8.
17. Codd AM, Choudhury B. Virtual reality anatomy: is it comparable with
traditional methods in the teaching of human forearm musculoskeletal
anatomy? Anat Sci Educ. 2011;4(3):119 –25.
18. Birbara NS, Sammut C, Pather N. Virtual reality in anatomy: a pilot study
evaluating different delivery modalities. Anat Sci Educ. 2020;13(4):445–57.
19. Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, Zhu H, Yao Y, Shui W, Shen Z,
Zhao J, Pan H. The role of three-dimensional printed models of skull in
anatomy education: a randomized controlled trail. Sci Rep. 2017;7(1):575.
20. Yammine K, Violato C. A meta-analysis of the educational effectiveness of
three-dimensional visualization technologies in teaching anatomy. Anat Sci
Educ. 2015;8(6):525–38.
21. Shui W, Zhou M, Chen S, Pan Z, Deng Q, Yao Y, Pan H, He T, Wang X. The
production of digital and printed resources from multiple modalities using
visualization and three-dimensional printing techniques. Int J Comput Assist
Radiol Surg. 2017;12(1):13–23.
22. Ryan JR, Chen T, Nakaji P, Frakes DH, Gonzalez LF. Ventriculostomy
simulation using patient-specific ventricular anatomy, 3D printing, and
hydrogel casting. World Neurosurg. 2015;84(5):1333–9.
23. Lo S, Abaker ASS, Quondamatteo F, Clancy J, Rea P, Marriott M, Chapman P.
Use of a virtual 3D anterolateral thigh model in medical education:
augmentation and not replacement of traditional teaching? J Plast Reconstr
Aesthet Surg. 2020;73(2):269–75.
24. Azer SA, Eizenberg N. Do we need dissection in an integrated problem-
based learning medical course? Perceptions of first- and second-year
students. Surg Radiol Anat. 2007;29(2):173–80.
25. Kerby J, Shukur Z, Shalhoub J. The relationships between learning outcomes
and methods of teaching anatomy as perceived by medical students. Clin
Anat. 2011;24(4):489–97.
26. Patel KM, Moxham BJ. The relationships between learning outcomes and
methods of teaching anatomy as perceived by professional anatomists. Clin
Anat. 2008;21(2):182–9.
27. Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality
for pediatric pain distraction during i.v. placement. CyberPsychol Behav.
2006;9(2):207–12.
28. Snelling J, Sahai A, Ellis H. Attitudes of medical and dental students to
dissection. Clin Anat. 2003;16(2):165–72.
29. Lee YH, Lee YM, Kwon S, Park SH. Reactions of first-year medical students to
cadaver dissection and their perception on learning methods in anatomy.
Korean J Med Educ. 2011;23(4):275–83.
30. Cook DA, Beckman TJ. Reflections on experimental research in medical
education. Adv Health Sci Educ Theory Pract. 2010;15(3):455–64.
31. Liu L, Zhou R, Yuan S, Sun Z, Lu X, Li J, Chu F, Walmsley AD, Yan B, Wang L.
Simulation training for ceramic crown preparation in the dental setting
using a virtual educational system. Eur J Dent Educ. 2020;24(2):199–206.
32. Silen C, Wirell S, Kvist J, Nylander E, Smedby O. Advanced 3D visualization in
student-centred medical education. Med Teach. 2008;30(5):e115–24.
33. Frendo M, Konge L, Caye-Thomasen P, Sorensen MS. Andersen SAW. A
Prospective, Controlled Cohort Study. Otol Neurotol: Decentralized Virtual Reality
Training of Mastoidectomy Improves Cadaver Dissection Performance; 2019.
34. Muller-Stich BP, Lob N, Wald D, Bruckner T, Meinzer HP, Kadmon M, Buchler MW,
Fischer L. Regular three-dimensional presentations improve in the identification
of surgical liver anatomy - a randomized study. BMC Med Educ. 2013;13:131.
35. Farra SL, Smith SJ, Ulrich DL. The student experience with varying immersion levels
of virtual reality simulation. Nurs Educ Perspect. 2018;39(2):99–101.
36. Khot Z, Quinlan K, Norman GR, Wainman B. The relative effectiveness of
computer-based and traditional resources for education in anatomy. Anat
Sci Educ. 2013;6(4):211–5.
37. Rudran B, Logishetty K. Virtual reality simulation: a paradigm shift for
therapy and medical education. Br J Hosp Med (Lond). 2018;79(12):666–7.
38. Sultan L, Abuznadah W, Al-Jifree H, Khan MA, Alsaywid B, Ashour F. An experimental
study on usefulness of virtual reality 360 degrees in undergraduate medical
education. Adv Med Educ Pract. 2019;10:907–16.
39. Tomlinson SB, Hendricks BK, Cohen-Gadol A. Immersive three-dimensional
modeling and virtual reality for enhanced visualization of operative
neurosurgical anatomy. World Neurosurg. 2019;131:313–20.
Publisher’sNote
Springer Nature remains neutral with regard to jurisdictional claims in
published maps and institutional affiliations.
Chen et al. BMC Medical Education (2020) 20:395 Page 10 of 10
