
ORIGINAL ARTICLE
Effect of Mandibular Advancement Surgery on Tongue Length
and Height and Its Correlation with Upper Airway Dimensions
N. K. Sahoo
1
•
Shiv Shankar Agarwal
2
•
Sanjeev Datana
2
•
S. K. Bhandari
1
Received: 22 August 2019 / Accepted: 16 April 2020
Ó The Association of Oral and Maxillofacial Surgeons of India 2020
Abstract
Introduction The spatial position and dimensions of oral
and pharyngeal soft tissues change post-mandibular
advancement (MA) surgery which involves changes in
position of soft palate, tongue and associated musculature.
There is no study which simultaneously evaluates changes
in tongue length and height post-MA surgery and correlates
these changes with changes in upper airway dimensions
and the amount of MA.
Materials and Methods Treatment records of 18 patients
that underwent MA with bilateral sagittal split ramus
osteotomy were evaluated at T1 (01 week before surgery)
and T2 (06 months post-surgery). Linear airway and ton-
gue measur ements were done on lateral cephalogram.
Mean volume and mean pharyngeal area values were
recorded from the acoustic pharyngometry (AP) records of
patients.
Results A statistically significant increase in tongue length
(P value \ 0.001) and nonsignificant change in tongue
height were observed at T2 ( P value[ 0.05). A statistically
significant increase in airway parameters recorded on both
lateral cephalogram and AP was observed at T2 (P value
\ 0.001). Correlation analysis did not show a statist ically
significant correlation of change in tongue length and
tongue height at T2 with the amount of MA, change in
airway parameters on lateral cephalogram and AP (P value
[ 0.05).
Conclusions Mandibular advancement surgery is a viable
option for improvement in pharyngeal airway in skeletal
Class II patients with retrognathic mandible. Changes in
tongue length observed in our study may correspond to the
stretch of protruders of tongue, especially genioglossus,
and may point toward possibl e relapse on a long-term
follow-up.
Keywords Mandibular advancement (MA) Obstructive
sleep apnea (OSA) Airway BSSRO
Introduction
Orthognathic surgeries involving maxilla and/or mandible
are mainly performed for bringing about positive
improvement in facial and smile aesthetics of the patient
apart from correction of various facial deformities [1, 2].
Maxillomandibular advancement by orthognathic surgery/
distraction osteogenesis (DO) is a well-documented treat-
ment modality for the management of obstructive sleep
apnea (OSA) secondary to hypoplastic/retr uded maxilla
and/or mandible. This treatment modality brings positive
improvement in airway by causing physical expansion of
the pharyngeal hard and soft tissues [3].
The surgeries involving mandibular setback (MS) are
well known to cause detrimental effects on upper airway
[4, 5]. The literature reveals that the spatial posi tion of oral
and pharyngeal soft tissues also changes post-surgery
which involves changes in the position of soft palate,
tongue and associated musculature [6, 7]. The surgeries
involving mandibular advancement (MA) cause forward
positioning of the tongue [4, 5]. This increases the
retropharyngeal airway space and may be helpful in indi-
viduals with compromised airway.
& N. K. Sahoo
1
Department of Oral and Maxillofacial Surgery, Armed Forces
Medical College, Pune, India
2
Department of Orthodontics and Dentofacial Orthopedics,
Armed Forces Medical College, Pune, India
123
J. Maxillofac. Oral Surg.
https://doi.org/10.1007/s12663-020-01375-2

Few studies have been reported in the literature docu-
menting the changes in tongue dimensions and position
post-surgery in MA cases [1, 2, 4, 8]. There is no study
which concurrently associates these tongue changes with
the altered pharyngeal airway dimensions and amount of
MA. Keeping this background in mind, the present study
was conducted to evaluate the changes in tongue height and
length post-MA surgery and simultaneously correlate these
changes with changes in upper airway dimensions.
Materials and Methods
Study Design
Retrospective analytical study.
Study Sample
This study was carried out at the Department of
Orthodontics and Dentofacial Orthopedics of a tertiary care
teaching institution. The study sample included treatment
records of 18 patients randomly selected from the institu-
tional archives that underwent MA surgery with bilateral
sagital split ramus osteotomy (BSSRO) between Jan 01,
2014, and Dec 31, 2016, and met the inclusion criteria of
the study. Lateral cephalogram used in this study was
recorded with a standardized technique using the same
machine (model: ADVAPX cephalostat machine, com-
pany: Panorraitic System, printer: Fujifilms DRY PIX
7000). Acoustic pharyngometry (AP) was used as a non-
invasive tool for evaluating and com paring area and vol-
umetric changes in airway post-surgery. AP for all patients
was recorded by the same operator with
ECCOVISION
Ò
Acoustic Pharyngometer
TM
using the
standard protocol.
Inclusion Criteria
1. Adult patients aged 18–28 years (both the sex).
2. Complete set of pre- and post-treatment orthodontic
records available with minimum 06-month follow-up.
3. The impacted mandibular third molars removed min-
imum 06 months prior to surgery.
4. Cases who underwent only MA with BSSRO surgery
without genioplasty.
5. Skeletal Class II cases with ANB C 4° and
overjet C 4 mm.
6. Nonextraction cases with crowding/spacing B 5 mm.
Exclusion Criteria
1. Cleft/syndromic/pat ients with neuromuscular disor-
ders/psychiatric patients.
2. Patients with history of recurrent pharyngeal infec-
tions, enlarged tonsils/adenoids, or any other medical
condition compromising airway.
3. History of previous ortho-surgical treatment or trauma
to jaw bones.
4. Presence of ankyloglossia or any other disorder
affecting tongue morphology and/or mobility.
Study Design and Data Collection
The selected cases (18 patients, 10 males and 08 females)
underwent MA with BSSRO surgery and were treated with
a standardized ortho-surgical treatment protocol at the
institute. Pre- and postsurgical orthodontics was carried out
using 0.022 MBT pre-adjusted edgewise appliance with
standard wire sequence protocol.
The lateral cephalogram and AP were recorded at two
time frames:
T1 01 week before surgery.
T2 06 months post-surgery.
The lateral cephalograms were manually traced, and
pharyngeal airway and tongue measurements were done at
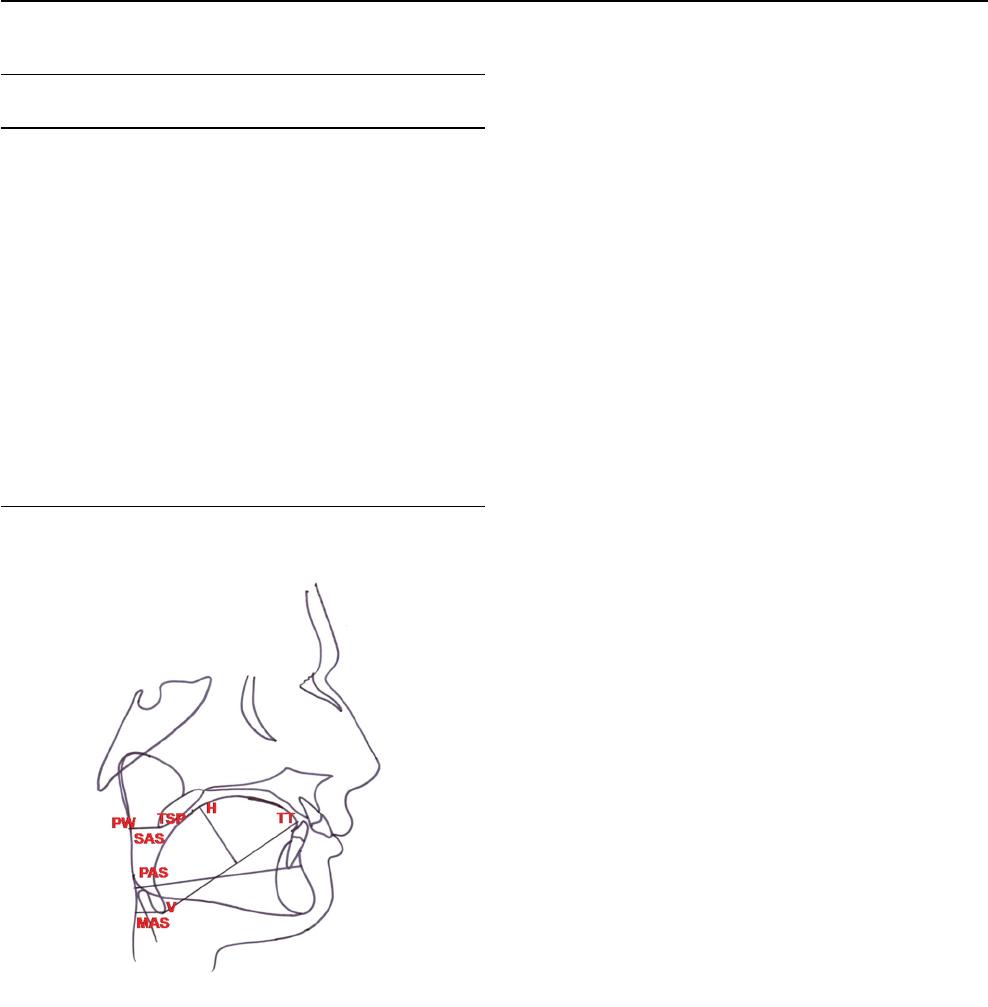
T1 and T2 (Table 1; Fig. 1). The pharyngeal airway
dimensions (mean volume and mean area) were recorded at
T1 and T2 from the AP records of the patients. The amount
of MA performed was recorded from the case sheets of the
patients. Changes in the above-mentioned parameters were
measured at T2 to know the changes in tongue and pha-
ryngeal airway dimensions post-surgery. The data were
collected and compiled in MS Excel work sheet and were
subjected to statistical analysis.
Statistical Analysis
The entire data were statistically analyzed using Statis tical
Package for Social Sciences (SPSS ver 21.0, IBM Corpo-
ration, USA) for MS Windows. The data on continuo us
variables were presented as mean and standard deviation
(SD). The statistical comparison of continuous variables
was done using paired t test. Pearson’s correlation was
carried out to study the correlations among the parameters
studied. The underlying normality assumption was tested
before subjecting each variable to t test and Pearson’s
correlation analysis. All the results are shown in tabular as
well as graphical format (using Box–Whisker plot) to
visualize the statistically significant difference more
clearly. In the entire study, the P values \ 0.05 were
J. Maxillofac. Oral Surg.
123
considered to be statistically significant. All the hypotheses
were formulated using two-tailed alternatives against each
null hypothesis (hypothesis of no difference).
Results
Post-surgical Changes in Parameters Studied
(Table 2)
The distribution of mean post-op (T2) tongue length
(70.56 mm, SD = 1.88 mm) was significantly higher
compared to mean pre-op (T1) tongue length (69.22 mm,
SD = 1.39 mm). The mean increase in tongu e length was
1.33 mm (SD = 0.87 mm), and this was statistically sig-
nificant (P value \ 0.001).
The distribution of mean post-op tongue height (29 mm,
SD = 1.58) did not differ significantly compared to mean
pre-op tongue height (29.33 mm, SD = 2.06 mm). The
mean decrease in tongue height was 0.33 mm with a SD of
1.50 mm, but this was not statistically significant (P value
[ 0.05).
The distribution of mean post-op airway parameters on
lateral cephalogram (SAS, PAS and MAS) was signifi-
cantly higher compared to mean pre-op airway parameters
(P value \ 0.001 for all).
The distribution of mean post-op parameters on AP
(mean volume and mean area) was significantly higher
compared to mean pre-op parameters (P value \ 0.001 for
all).
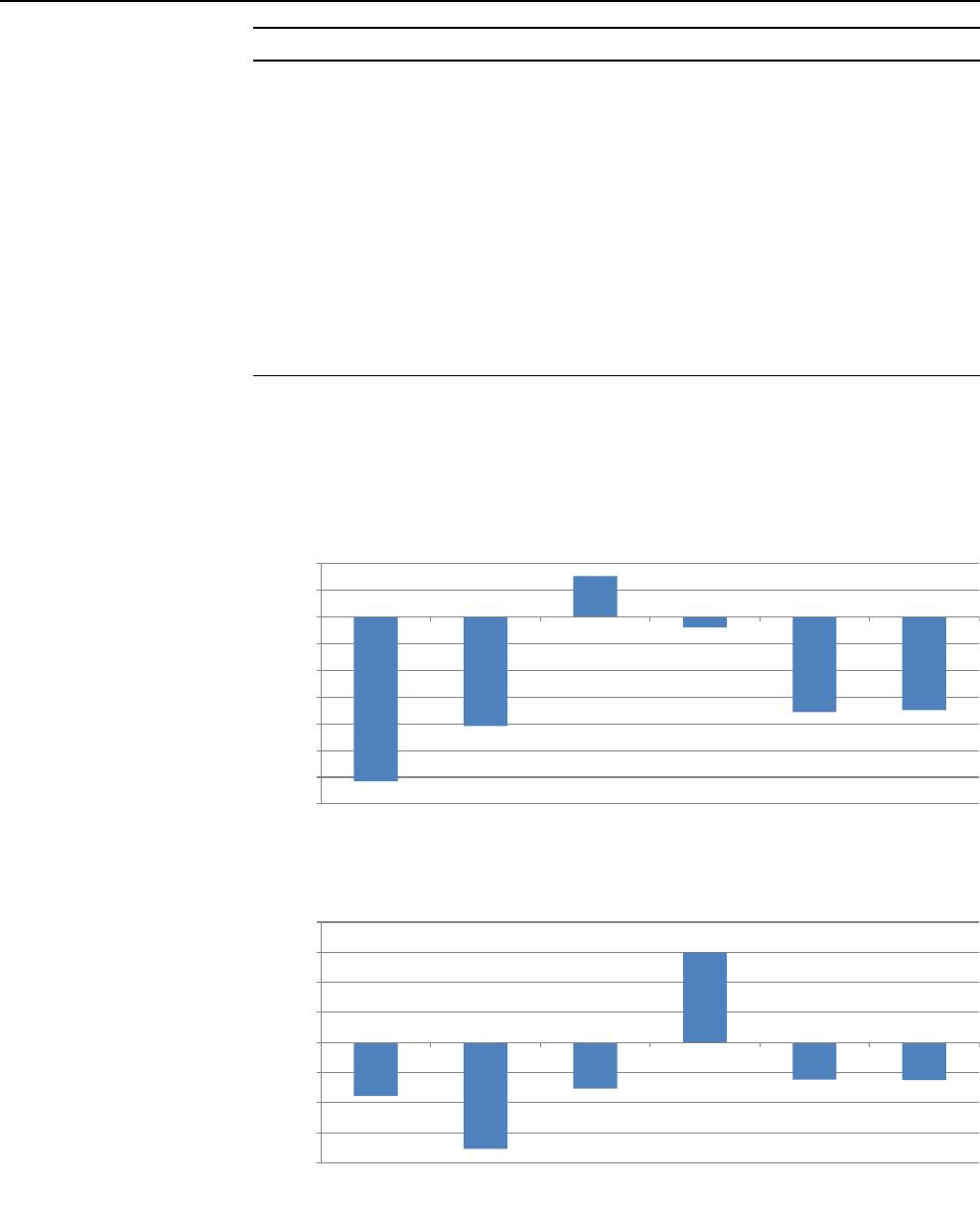
Correlation Analysis of Parameters Studied
with Change in Tongue Parameters (Table 3,
Figs. 2, 3)
The correlation analysis revealed that change in tongue
length (Fig. 2) and tongue height (Fig. 3) after surgery (at
T2) did not show statistically significant correlation with
the amount of MA, change in airway parameters (PAS,
SAS, MAS) on lateral cephalogram and change in AP
parameters (mean volume and mean area) in the study
sample (P value [ 0.05 for all).
Discussion
Various studies have demonstrated relationship of oral and
pharyngeal soft tissues with the craniofacial and dentofa-
cial structures. Any change in the skeletal tissues due to
growth, functional appliance therapy or orthognathic sur-
gery may cause spatial and dimensional changes in the
associated pharyngeal soft tissues (e.g., soft palate and
tongue) [9–12].
The tongue is an active and functional muscular organ
situated in the floor of the mouth. It is attached to the
lingual surface (genial tubercles) of the mandible, hyoid
bone, epiglottis and soft palate by various muscular
attachments [13, 14]. Various studies have shown that the
root of the tongue is more posteriorly positioned in skele-
tally class II subjects as compared to Class I and Class III
subjects. This compromises the pharyngeal airway, espe-
cially in the PAS and MAS region [14, 15]. MA causes
forward positioning of the tongue with a positive impact on
airway. This may also lead to changes in tongue dimen-
sions. Genioglossus muscle, which is the primary protruder
Table 1 Airway and tongue parameters studied on lateral
cephalogram
S.
no.
Parameter Measurement
1. Superior pharyngeal
airway space (SAS)
Linear distance measured from tip
of the soft palate (TSP) to the
nearest pharyngeal wall (PW)
2. Posterior airway space
(PAS)
Linear distance from posterior
margin of the base of the tongue
to the nearest pharyngeal wall on
Gonion-Point B (Go-B) line
3. Minimum/hypopharyngeal
airway space (MAS)
Minimum linear distance measured
from point V (intersection of
epiglottis and base of the tongue)
to the nearest pharyngeal wall
4. Tongue length (TL) Measured from point V to tip of the
tongue (TT)
5. Tongue height (TH) Perpendicular distance from the
highest point on the superior
surface of the tongue (H) to V-TT
line
Fig. 1 Landmarks used on lateral cephalogram
J. Maxillofac. Oral Surg.
123
muscle of the tongue, gets stretched during MA [16]. This
stretch may cause changes in tongue length and height, and
this may also be a cause of relapse in future. Based on these
inputs, this study was designed to evaluate the change s in
length and height of the tongue post-MA and also to find
correlation between these changes and airway parameters
assessed on lateral cephalogram and AP.
The literature reveals that lateral cepha logram is a reli-
able tool in determining airway dimensions [17, 18] with
efficacy comparable to computed tomography (CT) scans
[19]. A study [20] revealed that majority of the airway
landmarks can be reliably identified on a lateral cephalo-
gram. Also, it is routinely advised to all orthodontic
patients; hence, no additional cost and radiation exposure
are incurred to the patients. Therefore, lateral cephalogram
was used in our study to evaluate tongue and linear airway
dimensions.
AP is a noninvasive modality based on acoustic reflec-
tion technique for assessment of airway dimensions and
also to ascertain changes post-MA. It can be recorded chair
side at the orthodontic clinic, and its reliability is compa-
rable to CT scans [21]. Therefore, AP was used to assess
changes in mean volume and mean area in our study.
A statistically significant increase in tongue height on a
06-month follow-up after MA has been observed in one
study [22]. The change in tongue length was not statisti-
cally significant in this stud y at a 06-month follow-up.
These findings are not in agreement with our study wherein
a significant increase in tongue length has been observed
on a 06-month follow-up. The change in tongue height
was, however, not statistically significant in our study.
Prospective studies with a larger sample size may throw
more light in this regard.
Studies have shown that the tongue area remains
unchanged after the orthognathic surgery which provides a
more functional space to the tongue making it to assume a
more forward position [23]. This anterior positioning of the
tongue may be a reason for increased tongue leng th in our
study as the anterior portion of the tongue moves forward
during MA with stretching of the genioglossus mus cle.
The authors could not find any study which correlates
changes in tongue length and height with the amount of
MA. There is no literature available which correlates the
altered tongue dimensions post-MA with airway parame-
ters. AP was additionally used in our study to evaluate
changes in mean airway volume and area, and these
changes were also correlated with the altered tongue
dimensions. The correlation analysis revealed that change
in tongue length and height at T2 did not show statist ically
significant correlation with the amount of MA, change in
airway parameters on lateral cephalogram and changes in
mean volume and mean area evaluated by AP. A study [24]
observed mean anterior tongue displacement of 5.8 mm by
MA with DO and greater tongue displacement when DO
was accompanied with genioplasty. The tongue displace-
ment showed a strong correlation with the increase in PAS
width and anterior displacement of hyoid bone. A statisti-
cally significant increase in PAS and other linear, area and
volumetric parameters was also observed in our study at
T2. But in our study, the parameters were correlated with
tongue height and length rather than tongue displacement.
Table 2 Postsurgical changes in parameters studied
Parameter Mean SD
Tongue length (mm)
Pre-op 69.22 1.39
Post-op 70.56 1.88
P value
Pre versus post 0.002**
Tongue height (mm)
Pre-op 29.33 2.06
Post-op 29.00 1.58
P value
Pre versus post 0.524
NS
SAS (mm)
Pre-op 12.22 1.39
Post-op 13.22 1.56
P value
Pre versus post 0.003**
PAS (mm)
Pre-op 11.67 1.73
Post-op 13.56 1.81
P value
Pre versus post 0.002**
MAS (mm)
Pre-op 18.78 4.35
Post-op 20.06 4.45
P value
Pre versus post 0.013*
Mean vol (mm
3
)
Pre-op 25.11 5.04
Post-op 34.48 3.70
P value
Pre versus post 0.001***
Mean area (mm
2
)
Pre-op 2.53 0.51
Post-op 3.45 0.37
P value
Pre versus post 0.001***
Values are mean and SD, P values by paired t test
NS statistically nonsignificant
*P value \ 0.05; **P value \ 0.01; ***P value \ 0.001
J. Maxillofac. Oral Surg.
123
One study [25] observed no significant corr elation
between the pattern of tongue deformation on a dynamic
MRI and craniofacial structures (changes in tongue
volume, changes in airway volume and changes in SNA
and SNB angles). These results are similar to our study,
except that AP and lateral cepha logram were used to
Table 3 Correlation analysis of
parameters studied with change
in tongue parameters
Tongue parameter Correlation with r value P value
Change in tongue length Amount of advancement - 0.615 0.078
NS
Change in SAS - 0.408 0.275
NS
Change in PAS 0.152 0.697
NS
Change in MAS - 0.040 0.919
NS
Change in mean volume - 0.356 0.347
NS
Change in mean area - 0.349 0.357
NS
Change in tongue height Amount of advancement - 0.178 0.647
NS
Change in SAS - 0.354 0.351
NS
Change in PAS - 0.153 0.694
NS
Change in MAS 0.300 0.432
NS
Change in mean volume - 0.123 0.752
NS
Change in mean area - 0.125 0.749
NS
Correlation analysis by Pearson’s method
NS statistically nonsignificant
P value \ 0.05 is considered to be statistically significant correlation
*P value \ 0.05; **P value \ 0.01; ***P value \ 0.001
-0.615
-0.408
0.152
-0.04
-0.356
-0.349
-0.7
-0.6
-0.5
-0.4
-0.3
-0.2
-0.1
0
0.1
0.2
Amount of
advancement
Change in SAS Change in PAS Change in MAS Change in Mean
volume
Change in Mean
area
Pearson's r-value
Correlaon Analysis With Change in Tongue Length
Fig. 2 Correlation analysis of
parameters studied with change
in tongue length
-0.178
-0.354
-0.153
0.3
-0.123
-0.125
-0.4
-0.3
-0.2
-0.1
0
0.1
0.2
0.3
0.4
Amount of
Advancement
Change in SAS Change in PAS Change in MAS Change in Mean
volume
Change in Mean
area
Pearson's r-
value
Correlaon Analysis With Change in Tongue Height
Fig. 3 Correlation analysis of
parameters studied with change
in tongue height
J. Maxillofac. Oral Surg.
123

evaluate airway instead of dynamic MRI and these
parameters were correlated with changes in tongue height
and length instead of tongue deformation. Changes in SNA
and SNB angles were not evaluated in our study.
Conclusions
From the findings of this study, it can be concluded that
expansion of the skeletal tissues shows corresponding
changes in the oropharyngeal soft tissues. Mandibular
advancement surgery is a viable option for improvement in
pharyngeal airway in skeletal Class II patients with ret-
rognathic mandible. The changes in tongue length observed
in our stud y may correspond to the stretch of protruders of
the tongue, especially genioglossus, and may point toward
relapse on a long-term follow-up. Prospective studies with
a larger sample size and a long-term follow-up are required
to validate the findings of this study.
Compliance with Ethical Standards
Conflict of interest The authors declare that they have no competing
interests.
Ethics Statement The study design was approved by the institutional
ethical committee.
References
1. Eggensperger N, Smolka W, Iizuka T (2005) Long term changes
of hyoid bone position and pharyngeal airway size following
mandibular setback by sagittal split ramus osteotomy. J Cranio
Maxillo Fac Surg 33:111–117
2. Sahoo NK, Roy ID, Kulkarni V (2018) Mandibular setback and
its effects on speech. Oral Maxillofac Surg Cases. https://doi.org/
10.1016/j.omsc.2018.10.001
3. Zaghi S, Holty CEJ, Certal V et al (2016) Maxillomandibular
advancement for treatment of obstructive sleep apnea: a meta-
analysis. JAMA Otolaryngol Head Neck Surg 142(1):58–66
4. Marsan G, Oztas E, Cura N, Kuvat SV, Emekli U (2010) Changes
in head posture and hyoid bone position in Turkish Class III
patients after mandibular setback surgery. J Cranio Maxillo Fac
Surg 38:113–121
5. Chen F, Terada K, Hua Y, Saito I (2007) Effect of bimaxillary
surgery and mandibular setback surgery on pharyngeal airway
measurements in patients with class III skeletal deformities. Am J
Dentofac Orthop 131:372–377
6. Guven O, Saracoglu U (2005) Changes in pharyngeal airway
space and hyoid bone positions after body ostectomies and
sagittal split ramus osteotomies. J Craniofac Surg 16:23–30
7. Hasebe D, Kobayashi T, Hasegawa M et al (2011) Changes in
oropharyngeal airway and respiratory function during sleep after
orthognathic surgery in patients with mandibular prognathism. Int
J Oral Maxillofac Surg 40:584–592
8. Yoshida K, Rivera GA, Matsuo N et al (2000) Long-term prog-
nosis of BSSO mandibular relapse and its relation to different
facial types. Angle Orthod 70:220–226
9. Tangugsorn V, Skatvedt O, Krogstad O, Lyberg T (1995)
Obstructive sleep apnea: a cephalometric study. Part I. Cervico-
craniofacial skeletal morphology. Eur J Orthod 17:45–56
10. Tsuchiya M, Lowe AA, Pae EK, Fleetham JA (1992) Obstructive
sleep apnea subtypes by cluster analysis. Am J Orthod Dentofac
Orthop 101:533–542
11. Kaur S, Rai S, Sinha A, Ranjan V, Mishra D, Panjwani S (2015)
A lateral cephalogram study for evaluation of pharyngeal airway
space and its relation to neck circumference and body mass index
to determine predictors of obstructive sleep apnea. J Indian Acad
Oral Med Radiol 27:2–8
12. Turvey TA, Hall DJ (1984) Alteration in nasal airway resistance
following superior repositioning of the maxilla. Am J Orthod
Dentofac Orthop 45:109–114
13. Zhou L, Zhao Z, Lu D (2000) The analysis of the changes of
tongue shape and position, hyoid position in Class II, division 1
malocclusion treated with functional appliances (FR-I). Hua Xi
Kou Qiang Yi Xue Za Zhi 18(2):123–125
14. Tseng Y, Wu J, Chen C, Hsu K (2017) Correlation between
change of tongue area and skeletal stability after correction of
mandibular prognathism. Kaohsiung J Med Sci. https://doi.org/
10.1016/j.kjms.2017.03.008
15. Yamaoka M, Furusawa K, Uematsu T, Okafuji N, Kayamoto D,
Kurihara S (2003) Relationship of the hyoid bone and posterior
surface of the tongue in prognathism and micrognathia. J Oral
Rehabil 30:914–920
16. Takahashi S, Kuribayashi G, Ono T, Ishiwata Y, Kuroda T (2005)
Modulation of masticatory muscle activity by tongue position.
Angle Orthod 75:35–39
17. Malkoc S, Usumez S, Nur M, Donaghy CE (2005) Reproducibility
of airway dimensions and tongue and hyoid positions on lateral
cephalograms. Am J Orthod Dentofac Orthop 128:513–516
18. Aboudara C, Nielsen I, Huang JC, Maki K, Miller AJ, Hatcher D
(2009) Comparison of airway space with conventional lateral
headfilms and 3 dimensional reconstruction from cone beam com-
puted tomography. Am J Orthod Dentofac Orthop 135:468–479
19. Riley RW, Powell NB, Guilleminault C (1990) Maxillary,
mandibular, and hyoid advancement for treatment of obstructive
sleep apnea: a review of 40 patients. J Oral Maxillofac Surg
48:20–26
20. Miles PG, O’Reilly M, Close J (1995) The reliability of upper
airway landmark identification. Aust Orthod J 14:3–6
21. Agarwal SS, Jayan B, Kumar S (2015) Therapeutic efficacy of a
hybrid mandibular advancement device in the management of
obstructive sleep apnea assessed with acoustic reflection tech-
nique. Indian J Dent Res 26:86–89
22. Achilleos S, Krogstad O, Lyberg T (2000) Surgical mandibular
advancement and changes in uvuloglossopharyngeal morphology
and head posture: a short- and long-term cephalometric study in
males. Eur J Orthod 22:367–381
23. Turnbull NR, Battagel JM (2000) The effects of orthognathic
surgery on pharyngeal airway dimensions and quality of sleep.
J Orthod 27:235–247
24. Sriram SG, Andrade NN (2014) Cephalometric evaluation of the
pharyngeal airway space after orthognathic surgery and distrac-
tion osteogenesis of the jaw bones. Indian J Plast Surg
47:346–353
25. Lowth A, Juge L, Knapman F et al (2018) Dynamic MRI tongue
deformation patterns during mandibular advancement and asso-
ciations with craniofacial anatomy in OSA. J Sleep Res. https://
doi.org/10.1111/jsr.169_12766
Publisher’s Note Springer Nature remains neutral with regard to
jurisdictional claims in published maps and institutional affiliations.
J. Maxillofac. Oral Surg.
123
