
Editorial
A COVID-19 Airway Management Innovation with Pragmatic Efficacy
Evaluation: The Patient Particle Containment Chamber
LAUREN M. MALONEY ,
1,2
ARIEL H. YANG
,
2,3
RUDOLPH A. PRINCI,
1
ALEXANDER J. EICHERT,
2
DANIELLA R. HE
´
BERT,
4
TAELYN V. KUPEC,
7
ALEXANDER E. MERTZ,
5
ROMAN VASYLTSIV,
2,8
THEA M. VIJAYA KUMAR,
4
GRIFFIN J. WALKER,
6
EDDER J. PERALTA,
1
JASON L. HOFFMAN,
1
WEI YIN,
2
and CHRISTOPHER R. PAGE
2,9
1
Department of Emergency Medicine, Stony Brook University Hospital, Stony Brook, NY, USA;
2
Department of Biomedical
Engineering, Stony Brook University, Stony Brook, NY, USA;
3
Renaissance School of Medicine at Stony Brook University,
Stony Brook, NY, USA;
4
Department of Mechanical Engineering, Stony Brook University, Stony Brook, NY, USA;
5
School of
Health Technology and Management, Stony Brook University, Stony Brook, NY, USA;
6
Department of Technology and
Society, Stony Brook University, Stony Brook, NY, USA;
7
Department of Psychology, Stony Brook University, Stony Brook,
NY, USA;
8
Department of Physics and Astronomy, Stony Brook University, Stony Brook, NY, USA; and
9
Department of
Anesthesiology, Stony Brook University Hospital, Stony Brook, NY, USA
(Received 11 August 2020; accepted 17 August 2020)
Associate Editor Dan Elson oversaw the review of this article.
Abstract—The unique resource constraints, urgency, and
virulence of the coronavirus disease 2019 pandemic has
sparked immense innovation in the development of barrier
devices to protect healthcare providers from infectious
airborne particles generated by patients during airway
management interventions. Of the existing devices, all have
shortcomings which render them ineffective and impractical
in out-of-hospital environments. Therefore, we propose a
new design for such a device, along with a pragmatic
evaluation of its efficacy. Must-have criteria for the device
included: reduction of aerosol transmission by at least 90%
as measured by pragmatic testing; construction from readily
available, inexpensive materials; easy to clean; and compat-
ibility with common EMS stretchers. The Patient Particle
Containment Chamber (PPCC) consists of a standard
shower liner draped over a modified octagonal PVC pipe
frame and secured with binder clips. 3D printed sleeve
portals were used to secure plastic sleeves to the shower liner
wall. A weighted tube sealed the exterior base of the chamber
with the contours of the patient’s body and stretcher. Upon
testing, the PPCC contained 99% of spray-paint particles
sprayed over a 90s period. Overall, the PPCC provides a
compact, affordable option that can be used in both the in-
hospital and out-of-hospital environments.
Keywords—COVID-19, Aerosol, Intubation, Airway, Per-
sonal protective equipment, Emergency medical services.
ABBREVIATIONS
COVID-19 Coronavirus disease 2019
EMS Emergency medical services
HEPA High efficiency particulate air
NIOSH National Institute of Occupational
Safety and Health
PPCC Patient Particle Containment
Chamber
PPE Personal protective equipment
PVC Polyvinyl chloride
SARS-CoV-2 Severe acute respiratory syndrome
corona virus 2
Address correspondence to Lauren M. Maloney, Department of
Emergency Medicine, Stony Brook University Hospital, Stony
Brook, NY, USA. Electronic mail: lauren.maloney@
stonybrookmedicine.edu
Annals of Biomedical Engineering (Ó 2020)
https://doi.org/10.1007/s10439-020-02599-6
BIOMEDICAL
ENGINEERING
SOCIETY
Ó 2020 The Author(s)

INTRODUCTION
Recent evidence has shown that severe acute respi-
ratory syndrome corona virus 2 (SARS-CoV-2) may
remain infectious as an aerosol for at least 3 h.
29
Al-
though the exact mode of SARS-CoV-2 transmission
remains is still under investigation, it is likely that
airborne transmission via aerosols and droplets is a
significant factor in human-to-human spread.
31
Given
that the coronavirus disease 2019 (COVID-19) caused
by SARS-CoV-2 is predominantly a pulmonary dis-
ease,
1,22
it follows that moderately to severely ill
patients will often require some form of airway inter-
vention.
6,23
Secretions coming from the upper and
lower airways have been found to contain high viral
loads.
24,30
Therefore, aerosol-generating airway inter-
ventions such as ventilations with a bag-valve mask,
endotracheal intubation and extubation, as well as
tracheal suctioning place healthcare providers at
increased risk for viral exposure.
7,11,26
This risk of
exposure is further complicated by a widespread con-
cern about the availability of and access to appropriate
personal protective equipment (PPE).
3,25
Therefore,
innovative approaches to protect healthcare providers
from aerosols and droplets gen erated during airway
interventions is an integral component of limiting the
spread of the SARS-CoV-2 virus.
In late March 2020, Taiwanese anesthesiologist Dr.
Lai Hisen-Yung began to develop the Aerosol Box: a
transparent acrylic box to be placed over a patient,
with an open side facing the chest and two holes
through which a healthcare provider can insert their
hands in order to perform airway interventions.
13,15,27
A simulated patient cough using compressed oxygen to
explode a dye-containing balloon suggested that
without the Aerosol Box, dye dro plets were visible on
the healthcare provider’s face, torso, and floor, com-
pared to just the healthcare provider’s hands and
forearms with the Aerosol Box in place.
8
This barrier
device was rapidly adopted by hospitals internationally
even wi thout adequate evidence about its efficacy. This
was due in large part to dissemination via social media
sharing.
10,27
However, difficulties with the Aerosol Box were
soon realized. It was found to be restrictive, can cre-
ate tears in healthcare provider s’ PPE, interferes with
the use of a video laryngoscope, an d is subject to glare
from overhead lighting. In addition, it has a very
limited ability to adapt to healthcare provider height or
to patient body habitus.
8,10,18,28
Additional obstacles
include managing the device’s weight and bulkiness
during transport, securing the device to the bed espe-
cially if the head is elevated, and proper decontami-
nation and storage procedures.
10
Although multiple
iterations of the Aerosol Box have been devised
addressing some of these concerns, very limited overall
data exists to quantify its ability to protect staff present
in the patient’s room.
The use of barrier devices to limit airborne trans-
mission during airway interventions so far has been
limited to in-hospital sett ings. Many of the critiques of
the Aerosol Box would likely be amplified in an out-of-
hospital environment. This is due to the constraints of
ambulance stretcher dimensions, portability, and
storage. Additionally, the patient care compartment of
an ambulance is generally much smaller than a critical
care procedure room in an Emergency Department,
operating room, or inpatient hospital room. Perform-
ing airway interventions for patients suspected of
having coronavirus disease 2019 (COVID-19) in an
ambulance in accordance with current consensus rec-
ommendations
7,11
is further complicated by patient
compartments rarely being equipped to induce nega-
tive-pressure, and the lack of national standards for
ambulance ventilation systems in the United States.
20
Our primary objective was to create a barrier device
with the ability to reduce transmission of airborne
particles generated during airway interventions that is
portable and could be assembled from commonly
available components that are unlikely to be in short
supply during the pandemic. Critical design criteria for
the device included the reduction of transmission of
airborne particles by at least 90% as measured by
pragmatic testing; construction using materials outside
of the traditional hospital supply chain which can be
readily obtained on a limited budget and timeline; any
reusable components are easy to clean; and dimensions
allowing for use within the limit ed space of commonly
used EMS stretchers.
MATERIALS AND METHODS
Setting
This device was created and pragmatically tested at
Stony Brook University Hospital, in Stony Brook,
NY, USA. Stony Brook University Hospital is a sub-
urban, academic tertiary care center, located on a
shared campus with Stony Brook University.
Patient Particle Containment Chamber (PPCC)
Supplementary Material A describes the assembly
process in detail. Briefly, as illustrated in Fig. 1, the
PPCC frame was constructed from ½ in. PVC pipes
and PVC fittings (Fig. 1). A clear shower liner was
draped over the frame and secured in place using 2 in.
binder clips. 3D printed portals were used to mount
BIOMEDICAL
ENGINEERING
SOCIETY
MALONEY et al.
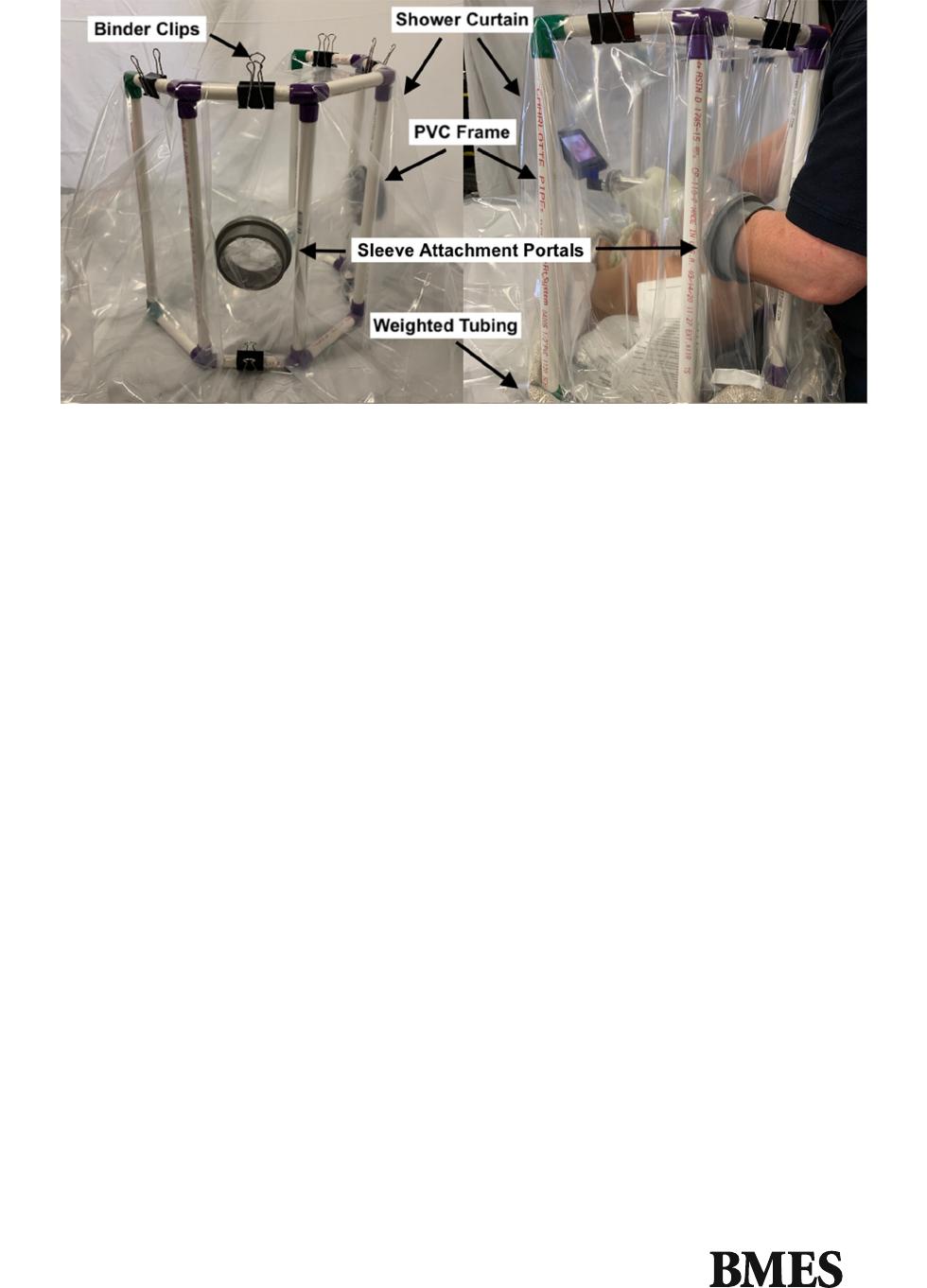
plastic sleeves onto the shower liner wall. Seven-inch
diameter 3mil poly tubing was used for the plastic
sleeve material. A weighted tube was draped along the
exterior base of the chamber and secured in place using
double sided tape.
Contamination Evident Chamber
A cube-shaped support structure was assem bled
using ½ in. 92 in. 948 in. poplar boards. The cube
was lined using 48 in. wide easel paper, creating the
Contamination Evident Chamber.
An investigator placed a gowned arm into the
Containment Evident Chamber via a small hole cut in
the easel paper and sprayed a can of black spray paint
within the chamber in all directions for 90 s. Paint was
visually seen on all six surfaces after the 90 s. The paint
was allowed to dry. This served as the control to
compare to the performance of the PPCC to.
The paper of the chamber was changed, and the
PPCC was placed within it. An identical can of black
spray paint was placed inside the PPCC and was
sprayed in all directions for 90 s by the same investi-
gator as before. The paint was allowed to dry.
Measurements
After being cut into 8.5 9 11’’ sections, the easel
paper was scanned into a digital image. ImageJ soft-
ware (NIH, Bethesda, MD) was then used to determine
the surface area covered by black paint. The total area
of paint coverage was measured in terms of pixels and
then converted to units of square inches using the
appropriate conversion factors.
RESULTS
Without the PPCC in place, the total surface area of
the Contamination Evident Chamber covered by black
paint was 2312 square inches. With the PPCC in place,
less than 1 square inch of surface area outside of the
PPCC was covered by black paint, and it was limited
to only the floor surface of the Contamination Evident
Chamber. The area of the Contamination Evident
Chamber underneath the PPCC, as well as the inner
surfaces of the walls of the PPCC, were completely
covered in black paint. The exact margins of the PPCC
were difficult to ascertain, as the folds of the shower
liner material draped onto the floor in an irregular
shape, as intended, and often in several layers. By
geometry, the PPCC frame covers 232 square inches of
the floor surface of the Contamination Evident
Chamber. Conservatively factoring in a possible 10%
additional surface area that may be covered by the
layers of shower liner, approximately 256 square inches
of the floor surface of the Contamination Evident
Chamber is covered by the PPCC. Reducing this area
from the total surface area of the Contamination
Evident Chamber covered in black paint without the
PPCC in place infers that 2,056 square inches of paint
covered area was outside the area encapsulated by the
PPCC. Therefore, the PPCC reduced the total surface
area of black paint in the Contamination Evident
Chamber by more than 99%.
The total cost per PPCC was $63.70. This fig ure in-
cludes the cost of shippi ng for products purchased
online, as well as the local sales tax of 8.6%. The cost
of the re-usable components was $52.18. The cost for
the single-use disposable components was $11.52. Of
FIGURE 1. The Patient Particle Containment Chamber with labeled components.
BIOMEDICAL
ENGINEERING
SOCIETY
COVID Patient Particle Containment Chamber

note, this does not include the cost of labor or the 3D
printing materials.
DISCUSSION
In response to the need for innovative ways to safely
perform airway interventions on patients with COV-
ID-19 in the setting of limited availability of personal
protective equipment, we designed a Patient Particle
Containment Chamber. The device was made from
readily available materials that are outside the tradi-
tional hospital supply chain. Total materials cost was
approximately $60. In comparison, commercially-
made solutions available for online purchase range in
cost from $60-270 (excluding tax and shipping costs),
and are dependent upon specific companies’ material
production and their supply availability.
16,17,19,27
Pragmatic testing of the chamber using a can of black
spray paint suggests that it is at least 99% effective in
reducing the transmission of small airborne particles.
The creation and subsequent almost immediate
world-wide adoption of the Aerosol Chamber was a
clear demonstation of the power of idea dissemination
through social media. However, the wildfire spread of
the device was followed by abrupt critiques about its
functionality, illustrating the cautionary tale proposed
by Duggan et al., for which they proposed the term
‘‘MacGyver bias.’’
12
The MacGyver bias is ‘‘the
inherent attraction of our own personal improvised
devices. This leads to a tendency to hold them in high
regard despite the relative absence of evidence for their
efficacy.’’
12
While necessity, especially when faced with
a highly contagious pandemic, may very well be the
mother of all invention, it is crucial that thought is
given to the determination of whether or not the device
does indeed do what is intended. Homemade devices
may come from a lack of existence of or lack of access
to a suitable commercially-available device. In such
cases, it is important to ponder how and if an inno-
vative solution would have undergone iterative chan-
ges in order to meet regulatory safety standar ds. Given
the speed with which COVID-19 traversed the globe,
traditional innovation timelines have been markedly
shortened. Adding to this, has been disruption of
hospital supply chains, leading to rapid depletion of
PPE. Furthermore, well-intentioned clinicians creating
these temporary solutions may lack a background in
the medical device innovation process. This may in-
crease the possibility of oversights in areas including
safety mechanisms, material selection, design toler-
ance, and product testing.
While the pragmatic testing of our proposed
chamber in reduction of airborne particle transmission
would certainly not conform to NIOSH standards, we
believe using a can of black spray paint is a reasonable
demonstration of efficacy. Reports suggest that air-
borne particles generated by standard spray paint cans
are of a size comparable to that which is necessary to
be defined as an infectious aerosol particle.
14,21
Fur-
thermore, this technique for testing can be easily
replicated by others if they would like to evaluate the
efficacy of their own de vices for a cost of less than $5.
Quantitative image analysis suggested that the de-
vice was able to prevent almost all simulated aero-
solized particles from leaving the device. Existing
published descriptions of attempts to evaluate how
useful barrier devices are at containing airborne par-
ticles have been limited to a qualitative description of
fluorescent dy e splatter patterns
8
and a video anlysis of
white vapor clouds flowing out of the Aerosol Box.
28
A
quantitative approach was described in the evaluat ion
of the utilit y of a constant flow canopy, a flexible
polyethylene canopy that is placed over the head and
upper thorax of pa tient while in a hospital bed which
contains a fan filtering unit and HEPA filter.
2
How-
ever, this device is not designed to allow an y sort of
airway intervention, but rather could limit the ambient
release of aerosols from patients undergoing noninva-
sive ventilation support. As smoke was piped under the
canopy, the face velocity and direction of the smoke
movement was determined, while photometry was used
to evaluate the integrity of the HEPA filter.
2
A single simulation-based study has been published
evaluating the impact of two generations of Aerosol
Boxes on sim ulated end otracheal intubation by anes-
thesiologists; however, it was not structured to evalu-
ate the efficacy of such devices on reducing airborne
particle exposure to clinicians.
5
It was found that with
the Aerosol Box in place, anesthesiologists took longer
to intubate, had fewer successful first attempts,
increased provider cognitive load , and increased pro-
vider discomfort during the procedure. Most con-
cerningly, was the number of breaches in PPE that
resulted from the gown getting stuck or torn in the arm
holes of the Aerosol Box.
5
Having already undergone several iterations, we
have shown that our device successfully addresses
many of these issues. The Patient Particle Containment
Chamber provides plenty of space for unhindered
airway interventions such as using a handheld video
laryngoscope or airway adjuncts. When not in use, it
can be collapsed and stored easily. Reusable compo-
nents are easy to clean and disinfect. Additionally, it is
unlikely that gowns will be torn given the mobile
nature of the sleeve attachment portals. Although ac-
cess to a 3D printer is necessary to create the sleeve
attachment portals, news reports sugge st access to this
equipment is more univers al than ever before, partic-
ularly through local libraries and high schools.
4,9
BIOMEDICAL
ENGINEERING
SOCIETY
MALONEY et al.

Future iterations of the Patient Particle Contain-
ment Chamber will need to address several design
elements. First, in order to consider leaving this device
in place for extended periods of time to allow for
longer airway interventions such as a nebulized medi-
cation, hourly tracheal suctioning, or extubation,
determination of a safe time period that the device can
be used before ambient oxygen is depleted or carbon
dioxide accumulates must be made. A system similar
to the fan filtering unit and HEPA filter described by
Adir et al. could be considered in order to better
control air and particle flow.
2
This may also help
mitigate dangerous diffusion of aerosols contained
within the chamber into the surrounding air once the
device is removed. Alternatively, we have created a
miniature version of the sleeve attachment portal
which would allow for ventilator tubing to pass
through the chamber. These could be configured to
allow for a bag -valve mask to be attached to the
chamber to introduce supplemental oxygen, as well as
adapted to allow for any outflow to be filtered. Several
components of the chamber could be prepared in ad-
vance in order to shorten the assembly time, and it may
be useful to include elastic cord within the top and
bottom partial octagons of the frame to allow for
faster frame assembly. Availability of completely pre-
fabricated fittings may help to remove the need to glue
pieces together. Specific to its out-of-hospital use, the
chamber frame fits well on the top of the most com-
mon EMS stretchers, though additional stability could
be added by using a clamp to hold the bottom of the
frame to the stretcher mattress. This could reduce the
potential for the device to topple off of the patient
during transport or when the head of the stretcher is
raised. Finally, the chamber needs to undergo formal
compliance testing, similar to what is done for labo-
ratory ventilator hoods, before its efficacy can be
reported with precision.
This study was limited to a single attempt made to
pragmatically quantify the amount of black spray
paint that was apparent on the inner surfaces of a 4-
foot cube with and without the chamber in place. The
data that we are able to report is limited due to a lack
of ability to determine the exact edge of the enclosure.
The irregular, multilayered way the shower liner was
wrapped around the weighted tube did not allow for
clearly defined boundaries. The initial iteration used a
6 foot long dishwasher tube filled with water and oc-
cluded at each end as the weighted tube; while it ap-
peared to work, later iterations using pellet-filled 2 inch
wide 2 Mil poly tubing instead offered more compli-
ance across surface contours and easier use.
The current COVID-19 pandemic has demonstrated
the lack of devices available to ensure provider safety
during airway interven tions. The device described
provides a promising solution to help protect both
hospital and out-of-hospital providers during airway
interventions. In addition, the design of the Patient
Particle Containment Chamber prioritizes the use of
readily accessible and economically affordable parts in
order to avoid contributing to a shortage of hospital
equipment during surges of patients. While current
constraints prevent the device from being formally
tested, initial pragmatic evaluation using airborne
particle simulation and imaging analysis yields highly
promising results. Although the device may not solve
all current concerns about healthcare provider safety
against respiratory viral infections, the PPCC provides
an additional, more versatile option to help limit
transmission of SARS-CoV-2 during high risk airway
interventions.
ACKNOWLEDGMENTS
This project was funded by a grant from the 2019–
2020 State University of New York Research Seed
Grant Program, RFP #20-03-COVID, awarded to
Drs. Maloney, Page and Yin. The authors have no
additional financial conflicts of interest to disclose.
Additionally, the authors would like acknowledge the
efforts of undergraduate students Blerta Zeqiri, Andy
La and Hao Li.
OPEN ACCESS
This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits
use, sharing, adaptation, distribution and reproduction
in any medium or format, as long as you give appro-
priate credit to the original author(s) and the source,
provide a link to the Creative Commons licence, and
indicate if changes were made. The images or other
third party material in this article are included in the
article’s Creative Commons licence, unless indicated
otherwise in a credit line to the material. If material is
not included in the article’s Creative Commons licence
and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need
to obtain permission directly from the copyright
holder. To view a copy of this licence, visit http://crea
tivecommons.org/licenses/by/4.0/.
FUNDING
Funding was provided by Research Foundation for
the State University of New York (Grant Number
1160436).
BIOMEDICAL
ENGINEERING
SOCIETY
COVID Patient Particle Containment Chamber

ELECTRONIC SUPPLEMENTARY MATERIAL
The online version of this article (https://doi.org/10.
1007/s10439-020-02599-6) contains supplementary
material, which is available to authorized users.
REFERENCES
1
Ackermann, M., S. E. Verleden, M. Kuehnel, et al. Pul-
monary vascular endothelialitis, thrombosis, and angio-
genesis in COVID-19. N. Engl. J. Med. 383(2):120–128,
2020.
2
Adir, Y., O. Segol, D. Kompaniets, et al. COVID-19:
minimising risk to healthcare workers during aerosol-pro-
ducing respiratory therapy using an innovative constant
flow canopy. Eur. Resp. J. 55(5):1, 2020.
3
Artenstein, A. W. In pursuit of PPE. N. Engl. J. Med.
382(18):e46, 2020.
4
Balzer, C. Using 3D to make PPE: library resources help
create much-needed face shields. American Libraries Ma-
gazine.
5
Begley, J. L., K. E. Lavery, C. P. Nickson, D. J. Brewster.
The aerosol box for intubation in coronavirus disease 2019
patients: an in situ simulation crossover study. Anaesthe-
sia.n/a(n/a).
6
Bhatraju, P. K., B. J. Ghassemieh, M. Nichols, et al.
COVID-19 in critically ill patients in the seattle region -
case series. N. Engl. J. Med. 382(21):2012–2022, 2020.
7
Brewster, D. J., N. Chrimes, T. B. Do, et al. Consensus
statement: safe airway society principles of airway man-
agement and tracheal intubation specific to the COVID-19
adult patient group. Med. J. Aust. 212(10):472–481, 2020.
8
Canelli, R., C. W. Connor, M. Gonzalez, A. Nozari, and
R. Ortega. Barrier enclosure during endotracheal intuba-
tion. N. Engl. J. Med. 382(20):1957–1958, 2020.
9
Cardine, S. Good Samaritans borrow unused school
machines to 3D-print coronavirus masks, shields. Los
Angeles Times.
10
Chan, A. Should we use an ‘‘aerosol box’’ for intubation?
2020. https://litfl.com/should-we-use-an-aerosol-box-for-in
tubation/. Accessed 22 June 2020.
11
Cook, T. M., K. El-Boghdadly, B. McGuire, A. F.
McNarry, A. Patel, and A. Higgs. Consensus guidelines for
managing the airway in patients with COVID-19: Guide-
lines from the Difficult Airway Society, the Association of
Anaesthetists the Intensive Care Society, the Faculty of
Intensive Care Medicine and the Royal College of Anaes-
thetists. Anaesthesia. 75(6):785–799, 2020.
12
Duggan, L. V., S. D. Marshall, J. Scott, P. G. Brindley, and
H. P. Grocott. The MacGyver bias and attraction of
homemade devices in healthcare. Can. J. Anaesth.
66(7):757–761, 2019.
13
Everington, K. Taiwanese doctor invents device to protect
US doctors against coronavirus. Taiwan News. 23 Mar
2020.
14
Go
¨
hler, D., and M. Stintz. Granulometric characterization
of airborne particulate release during spray application of
nanoparticle-doped coatings. J. Nanoparticle Res.
16(8):2520, 2014.
15
Hsu, S. H., H. Y. Lai, F. Zabaneh, F. N. Masud. Aerosol
containment box to the rescue: extra protection for the
front line. Emerg. Med. J. 2020.
16
Intubation Box. https://www.vacep.org/intubationbox.
Accessed 22 June 2020.
17
IntubationPod. https://utwpods.com/products/intubation
pod. Accessed 24 June 2020.
18
Kearsley, R. Intubation boxes for managing the airway in
patients with COVID-19. Anaesthesia. 75(7):969, 2020.
19
Leyva Moraga, F. A., E. Leyva Moraga, F. Leyva Moraga,
et al. Aerosol box, an operating room security measure in
COVID-19 pandemic. World J. Surg. 44(7):2049–2050,
2020.
20
Lindsley, W. G., F. M. Blachere, T. L. McClelland, et al.
Efficacy of an ambulance ventilation system in reducing
EMS worker exposure to airborne particles from a patient
cough aerosol simulator. J. Occup. Environ. Hygiene
16(12):804–816, 2019.
21
Lindsley, W. G., J. S. Reynolds, J. V. Szalajda, J. D. Noti,
and D. H. Beezhold. A cough aerosol simulator for the
study of disease transmission by human cough-generated
aerosols. Aerosol. Sci. Technol. 47(8):937–944, 2013.
22
Madabhavi, I., M. Sarkar, N. Kadakol. COVID-19: a re-
view. Monaldi archives for chest disease = Archivio Mon-
aldi per le malattie del torace. 2020;90(2).
23
Meng, L., H. Qiu, L. Wan, et al. Intubation and ventilation
amid the COVID-19 outbreak: Wuhan’s experience. Anes-
thesiology. 132(6):1317–1332, 2020.
24
Setti, L., F. Passarini, G. De Gennaro, et al. Airborne
transmission route of COVID-19: why 2 meters/6 feet of
inter-personal distance could not be enough. Int. J. Envi-
ron. Res. Public Health 2020;17(8).
25
Shanafelt, T., J. Ripp, M. Trockel. Understanding and
addressing sources of anxiety among health care profes-
sionals during the COVID-19 pandemic. JAMA 2020.
26
Tran, K., K. Cimon, M. Severn, C. L. Pessoa-Silva, and J.
Conly. Aerosol generating procedures and risk of trans-
mission of acute respiratory infections to healthcare
workers: a systematic review. PLoS ONE. 7(4):e35797,
2012.
27
Tseng, J. Y., and H. Y. Lai. Protecting against COVID-19
aerosol infection during intubation. J. Chin. Med. Assoc.
83(6):582, 2020.
28
Turer, D. C., B. H. Jason. Intubation boxes: an extra layer
of safety or a false sense of security? STAT. 2020.
29
van Doremalen, N., T. Bushmaker, D. H. Morris, et al.
Aerosol and surface stability of SARS-CoV-2 as compared
with SARS-CoV-1. N. Engl. J. Med. 382(16):1564–1567,
2020.
30
Wang, W., Y. Xu, R. Gao, et al. Detection of SARS-CoV-2
in different types of clinical specimens. JAMA.
323(18):1843–1844, 2020.
31
Zhang, R., Y. Li, A. L. Zhang, Y. Wang, and M. J. Mo-
lina. Identifying airborne transmission as the dominant
route for the spread of COVID-19. Proc. Natl. Acad. Sci.
USA 117(26):14857–14863, 2020.
Publisher’s Note Springer Nature remains neutral with re-
gard to jurisdictional claims in published maps and institu-
tional affiliations.
BIOMEDICAL
ENGINEERING
SOCIETY
MALONEY et al.
